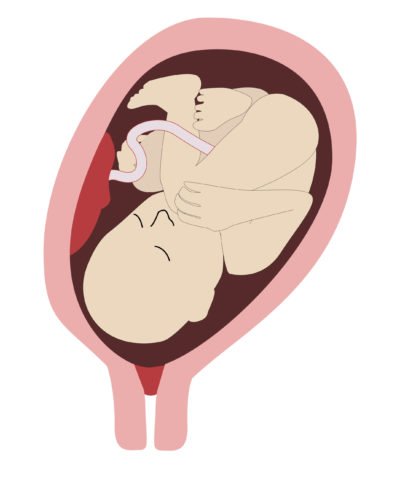
“Breech” means the baby is positioned to come out either bottom or feet first.
There Are 3 Main Types of Breech Presentation:
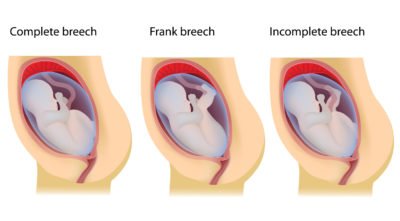
1. Complete Breech: Both knees are bent (with the bum and feet near the birth canal).
2. Frank Breech: Both legs are sticking straight up with the feet near the head (while the bum is aimed at the birth canal)
3. Incomplete Breech: one knee is bent (while the bum and foot are close to the birth canal).
Insider Info: There’s also a “Footling Breech” presentation in which one or both feet lie over the cervix. In this case, it’s possible (but highly unlikely), for a woman to go into labor and find a foot dangling out of her. As you’ve probably guessed, this situation warrants a call to the doc and an emergent trip to the hospital.
To Determine if Your Baby is Breech, Your Doctor Will Assess His/Her Position at Every Visit During the Second and Third Trimesters.
He/she will do this by feeling your belly. If your doc thinks that your baby is in a position other than head-down, face-down, toward the end of your pregnancy, then he/she will do an internal exam to feel for the head. He/she may also perform an ultrasound (to confirm the position).
Ok, My Baby is Breech. What Happens Next?
Obviously, coming out backwards isn’t recommended, so the baby needs to either: turn around him/herself, be turned around, or be born via C-section (or rarely, by vaginal delivery).
- The Good News: Many babies start out in the breech position but turn around toward the end of the pregnancy.
- The Not so Good News: If your baby has NOT turned around by 36 weeks, then he/she is probably stuck in the breech position.
If Your Baby Continues to Hang Out in The Breech Position, Your Doctor May Try to Turn Him/Her Around With An External Cephalic Version Maneuver. This maneuver is typically done around 37 weeks and works about 50% of the time.1 It does have some associated risks, though. Get Wise about External Cephalic Versions here.
If the External Cephalic Version Maneuver Doesn’t Work (Or Isn’t Attempted) And Your Baby Still Refuses to Get into a Favorable Position Him/Herself, Then You’re Probably Headed For a C-Section.
- A planned C-section is the preferred mode of delivery for persistently breech babies. As a result, 90% of breech babies are delivered via C-section.2
- There’s a growing trend, however, in which women with breech babies request to deliver vaginally. In rare cases, this can be attempted, but vaginal breech deliveries are associated with a higher rate of complications for both Mom-to-be and baby.3
- If you’re pregnant with twins and twin B (the twin who will be delivered second) is breech and twin A is head-down, face-down, then a vaginal delivery of both twins may be attempted (if this is what the doctor recommends).
Whew…Ok…Is There Anything Else I Should Know About Breech Babies?
Yes. Breech babies have a slightly higher risk of having a hip deformity called Developmental Hip Dysplasia (DDH). The hip socket, in this case, doesn’t fully cover the ball portion of the thigh bone (the femur), making the hip unstable.
Insider Info: First-born girls who were in a breech position in the womb (at 34 weeks or after) have the highest risk of developmental hip dysplasia, especially if DDH runs in their family.
The Good News:

Pediatricians are Always on the Lookout for Developmental Hip Dysplasia and Have Protocols in Place So They Don’t Miss It.
For Example…
- Pediatricians typically do a hip ultrasound at 4-6 weeks of life for the following babies:
- ALL babies who were breech at 34 weeks or after.
- Babies with a family history of DDH.
- Babies with an abnormal hip exam.
- Your baby’s pediatrician (or family medicine doctor) will check the stability of your baby’s hips at every office visit (until 1 year or so). Docs check the hips with 2 maneuvers: the Barlow & Ortolani maneuvers. To you it will look like the doc is doing yoga moves on your baby, but in reality, he/she is feeling for the characteristic “clunk” of an unstable hip.
- If your baby is born with developmental hip dysplasia, the problem can usually be fixed without surgery. Early diagnosis and intervention are key, though. If the hip remains unstable, then it will grow in an abnormal way, causing your child to develop a limp when he/she is older. If the issue is discovered early on, however, a harness can be used to coax the hip bone back into its socket so that it grows properly.
PediaTip: While your pediatrician should ask (or already know) if your baby was breech after 34 weeks of pregnancy, it’s always good to remind him/her just in case.
A Word About Transverse and Oblique Lies

What’s Are Transverse and Oblique Lies Again?
- A transverse lie means the developing baby is lying sideways in the womb. This position is seen in about 0.3% of term pregnancies (pregnancies that go to 37 weeks and beyond).4 It looks like this:
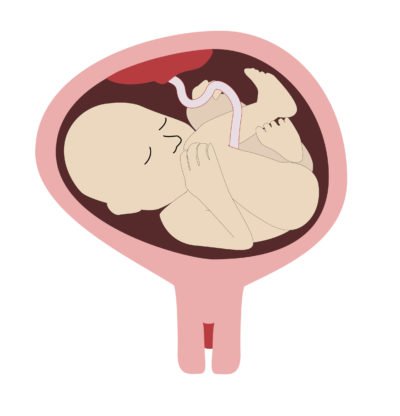
- An oblique lie is when the baby is lying in a diagonal position in the womb (see pic below).
- As with breech babies, most babies in transverse and oblique positions shift into the desired head-down, face-down position before 36 weeks.
- If your baby is still in a transverse or oblique position at 36 weeks, then an external cephalic version may be tried at 37 weeks (or after).
- If the external cephalic version doesn’t work and your baby continues to hang out in a transverse or oblique position, then delivery via C-section will be recommended when your baby is full term.
The Bottom Line
Most babies who’ve adopted a breech, transverse, or oblique position will move into the ideal head-down, face-down position by 36 weeks. If not, the doc may perform an external cephalic version maneuver to try to turn the baby around. If your baby remains stuck in a breech, sideways, or diagonal position at 36 weeks and the external cephalic version fails (or isn’t attempted in the first place), then a planned C-section will probably be recommended once the baby is full term. Get Wise(r) about C-Sections.