A “bone fracture” is the medical term for a broken bone. Broken bones in children are a bit trickier to manage than broken bones in adults because of kids’ growth plates.
What the Heck are Those? Growth plates are areas of cartilage at the ends of each bone. They’re important because they allow bones to grow longer. After a child goes through puberty, his/her growth plates fuse, signaling that he/she is done growing.
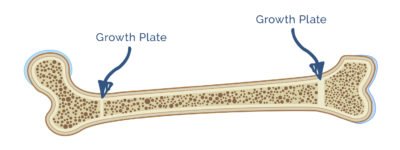
Doctors are super protective of growth plates and get all worked up if something like a bone break (aka a fracture) threatens to disrupt them. Why? Because a fracture of the growth plate can cause the affected limb to grow improperly and appear crooked or shorter than the opposite limb.
Although broken bones aren’t super common in toddlers, they need to be treated and managed by an orthopedic specialist (aka a bone doctor).
In this article, we’ll talk about the different types of fractures in kids, the signs that your child (might) need an X-ray, and how to care for a cast.
Fractures in Kids
There are 2 Main Types of Fractures in Kids:
1. Simple Fractures (aka “Closed Fractures”): Simple fractures are straightforward breaks in the bone. When there’s a simple fracture, the skin remains intact (meaning the broken bone doesn’t come through the skin).
2. Compound Fractures (aka “Open Fractures”): Compound fractures are bad breaks in which the end of the broken bone pokes through the skin. This type of fracture looks pretty gnarly and has a greater risk of getting infected than a simple fracture. Compound fractures must be treated with surgery.
Insider Info: A “displaced” fracture is a fracture in which the pieces of the fractured bone don’t line up properly. Displaced fractures can be either simple fractures OR compound fractures.
You Mentioned Something About Growth Plates and Fractures. Tell Me More…
As discussed above, each bone has 2 growth plates (one on either end), which enable the bone to grow longer. 15-30% of all childhood fractures involve the growth plate.1 Most aren’t serious, though, and don’t interfere with the growth of the affected body part.
Insider Info:
- The “Salter-Harris Fracture Classification System” is a fancy rating scale that ranks growth plate fractures by severity.
- A Salter-Harris Type 1 fracture represents a minor growth-plate fracture, whereas a Salter-Harris Type 5 fracture is the most severe. Fortunately, Salter-Harris Type 5 fractures aren’t all that common.
- If your child breaks a bone and the fracture goes through the growth plate, the doctor will let you know. This info won’t necessarily change the way the doctor manages the fracture, but it will dictate how careful your child needs to be during the healing process (and how psycho you need to be about shadowing him/her). As you can imagine, it’s often tough for toddlers (even ones with broken bones and casts) to follow the rules and take it easy during the recovery process.
What are the Symptoms of a Fracture?

If your toddler takes a spill and cries and holds his/her arm or leg afterwards, you may worry about a broken bone. It can be tough, however, to tell the extent of a musculoskeletal injury just by looking at the limb. Here are a few tips to help you determine when an X-ray might be necessary.
The Top 6 Signs That Your Child (Might) Need an X-Ray:
He/She:
1. Has Prolonged Crying and Pain. Expect your child to cry after an injury, but don’t expect the crying to go on and on.
2. Refuses to Move the Limb.
Insider Info: Kids are sometimes afraid to move their injured limb because they “remember” the pain they felt when they hurt it and don’t want to revisit that pain. Without forcing it, try to distract your child or give him/her a fun incentive to use the affected limb. If he/she still refuses to use it, you might have a fracture on your hands.
3. Refuses to Walk or Limps When He/She Walks.
4. Has Major Bruising and Swelling at the Site of the Injury.
5. Has a Limb That “Looks” Broken (i.e. That’s at a Weird Angle After the Injury).
6. Had a “Mechanism of Injury” That Often Results in Broken Bones.
For example, falling on an outstretched hand while trying to break a fall is a common cause of wrist fractures in kids.
Insider Info: If a child 2 years (or older) hurts his/her ankle, the doctor will use the “Ottawa Ankle Rules” to determine if he/she needs an X-ray. These rules take into account the location of the pain and the child’s ability to bear weight on the injured ankle.
In Addition to the Above Symptoms, There are Certain Signs That Doctors Look For on the Physical Exam to Help Them Determine if a Bone is Fractured (and Needs an X-Ray).
These Signs Include:
- Swelling.
- Tenderness.
- Deformity (i.e. the limb looks crooked).
- Poor circulation (i.e. the pulses are weak and hard to feel).
- Crepitus (i.e. there’s a crackling sensation under the skin that feels like pressing on bubble wrap. Crepitus is a sign that air is trapped in the tissue beneath the skin).
How are Fractures Diagnosed?

The Answer: With an X-ray of the affected body part.
Insider Info:
- Fractures (especially fractures involving the growth plate) can take a while to show up on X-ray. If your child is still complaining of pain after a negative X-ray, let the doctor know. In this case, your child may need a repeat X-ray OR require a higher-resolution image (such as a CT scan or an MRI) to make sure there isn’t a hidden fracture.
- X-rays are pretty good at diagnosing bone breaks. MRIs are best for soft-tissue injuries (which can present in the same way as a fracture).
How are Fractures Treated?
If the X-ray shows a fracture (or a fracture is suspected even though the X-ray is negative), the pediatrician (or the ER doctor) will refer your child to an orthopedic (bone) surgeon.
- If the fracture is minor, the orthopedic surgeon may just recommend a cast. Orthopedic surgeons often wait a few days for the swelling to go down before “casting” a broken bone. A splint can be applied in the meantime to keep the affected limb stable. The type of break determines how long the cast needs to stay on.
- If the fracture is “displaced” (i.e. if the pieces of the fractured bone don’t line up properly), the ends of the bone may need to be realigned (without surgery, in this case) before the cast is put on. The realigning process hurts like a mother and is often done in the Emergency Department after giving the patient a sedative, such as intranasal Versed (which goes up the nose).
- If the fracture is severe, surgery under anesthesia may be needed.
PediaTips for Cast Care

- Casts are made out of plaster or fiberglass. Fiberglass casts are lighter and more durable than plaster casts. They also come in different colors, which is a nice perk.
- Resist the temptation to put a pencil or a spoon down your child’s cast to relieve an itch.
Why? Because putting an object down there can mess with the padding inside, leading to increased pressure on the skin and possible skin breakdown (read: a wound).
- Use a cast cover or plastic wrap for baths and showers.
- Draw something fun on your kid’s cast.
- Periodically evaluate the injured body part after the cast has been put on. For example, make sure that your kiddo can still wiggle his/her fingers and that his/her pain isn’t worsening.
Why? Because docs are always on the lookout for compartment syndrome, a rare complication that can occur when a cast is too tight.
Tell Me More About “Compartment Syndrome”…
Compartment syndrome is caused by a buildup of pressure inside one of the enclosed muscle spaces under the cast. The increased pressure is caused by swelling or bleeding into the compartment where the muscles are located. The elevated pressure can slow the blood supply to the muscle and nerve cells, leading to serious problems.
What are the Symptoms of Compartment Syndrome?
Compartment Syndrome is Characterized by the 5 Ps:
1. Pain: Severe pain “out of proportion” to how the affected body part looks (i.e. it may seem like your child is being super dramatic about the pain, when he/she isn’t).
2. Pallor: Pale skin.
3. Paresthesia: Numbness and tingling.
4. Pulselessness: Diminished or absent pulses.
5. Paralysis: Trouble moving the affected limb (this is a late finding).
How is Compartment Syndrome Diagnosed?
If the orthopedic surgeon suspects that a child has compartment syndrome, he/she will stick a pressure gauge (i.e. a big *ss needle) into the affected limb to see if there’s a buildup of pressure inside the muscle compartment.
Note: From personal experience, this does NOT feel good.
How is Compartment Syndrome Treated?
With immediate surgery (to relieve the pressure).
The Good News: Compartment syndrome is RARE. Still, it doesn’t hurt to be on the lookout for it.
The Bottom Line
Doctors are especially cautious about bone fractures in kids because of their growth plates. Although most injuries in toddlers don’t result in broken bones, it’s worth calling the doctor if you’re worried about a possible fracture.