Welcome to Week 18 of Parenting Your Baby!
In This Week’s PediaGuide, We’ll Discuss:
- The Hot Topics for the Week, Including:
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

We’re coming up on 5 months. As you venture out more with your baby, they’ll naturally be exposed to a greater number of germs. The good news is that this exposure will help build up their immunity. The not so good news is they’ll probably get a few illnesses along the way. The Hot Topics for this week focus on one of these common illnesses (Croup) and on a symptom that’s commonly seen in the pediatric population (Wheezing).
Sleep:
Your baby continues to need about 12-15 hours of sleep per day (including naps).
Feeding:
The name of the game continues to be breast milk and/or formula.
If your baby’s doctor recommends that you introduce solid foods before 6-months of age, Get Wise about how to do it again, here.


As a Reminder, the Hot Topics for This Week Are:
Get Wise(r) About These Topics Below…
Disease Spotlight: Croup
Croup (fancy name: laryngotracheobronchitis) is a respiratory illness that causes a portion of the affected child’s airway (below the vocal cords) to become inflamed and narrowed. Think: Laryngitis in babies.
Croup is typically caused by a virus (such as the parainfluenza virus) and is most commonly seen in kids 6 months to 3 years of age.1
What are the Symptoms of Croup?
The Symptoms of Croup Include:
- Cold-Like Symptoms (such as a runny nose and a low-grade fever).
- A Hoarse Voice: Croup will make your child’s cries and coos raspy.
- A “Barking” Cough: A “barking” cough is a classic sign of croup. Your child will sound like a dog or a seal barking. You’ll know it when you hear it. The cough may be worse at night and when your child is crying.
- Inspiratory Stridor: Children with more pronounced cases of croup often make a high-pitched squeaking or whistling sound when they inhale.
- For moderate cases of croup, you may hear this sound (fancy name: inspiratory stridor) only when your child is upset.
- For more severe cases, the inspiratory stridor may be heard with every breath.
- Trouble Breathing: Respiratory distress is seen in severe cases of croup and is due to an intense narrowing of the upper airway. Babies, in this case, look like they’re huffing and puffing.
Insider Info:
- Days 2 and 3 of croup tend to be worse than Day 1, so call the doctor right away if you hear the classic barking cough.
- If you want to impress the doctor, you can casually mention the “Westley Croup Severity Score.”
What’s That? It’s a scoring system that gives doctors and nurses a sense of how bad the croup is and how aggressively they need to treat it. This scoring system evaluates 5 factors and can be used in kids under 6 years of age.
Get Wise(r) About the Westley Croup Severity Score, Here.
How is Croup Diagnosed?
Croup is usually diagnosed based on a child’s symptoms, with the barking cough being the telltale sign.
Insider Info: If your baby develops severe croup, the doctor may recommend that they get a neck X-ray in the ER to confirm the diagnosis and to rule out other possible causes of upper airway swelling. The classic neck X-ray finding for croup is the “steeple sign” (which shows the narrowing of the trachea – aka the windpipe). See how the upper part of the trachea looks like a church steeple in the pic below?
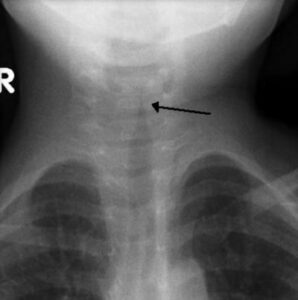
Image Source: Wikipedia
What Can Be Done to Treat Croup?
- Call the doctor ASAP if you think your child has croup.
- For mild to moderate cases of croup, the doctor will either prescribe an oral steroid (to take at home) OR give your child a steroid shot in the office to reduce the upper airway swelling. Sometimes a second steroid dose is needed the following day.
- In addition, you can put a humidifier in your baby’s room or take them into the bathroom and run a hot shower. The warm, moist air will help alleviate the airway swelling.
- For more severe cases of croup, a trip to the ER may be in order. In the ER, the doctor will give your child steroids and may administer a breathing treatment called racemic epinephrine to open up the airways.
Symptom Spotlight: Wheezing
Now, let’s turn our attention to another noise that can be heard with respiratory problems: wheezing.
What’s Wheezing?
Wheezing is a high-pitched whistling or squeaking sound that’s made when the airways become inflamed and narrowed. Although wheezing is best heard with a stethoscope, it may be heard with the naked ear in severe cases.
Insider Info: Parents often mistake “transmitted upper airway sounds” (the Dark Vader breathing you hear with a cold) for wheezing. If you’re not sure what you’re hearing, ask the doctor to take a listen.
What Causes Wheezing?
- Wheezing can be heard anytime the airways are inflamed or narrowed. For example it can be heard with colds & asthma, and when a foreign object (such as a coin or a toy) is swallowed.
- Wheezing with Colds: Some infants wheeze when they get a cold, especially when they have bronchiolitis, an infection of the small airways of the lower lungs.
Wheezing with colds doesn’t necessarily mean that a child is going to develop asthma (although it’s a possibility). In the pediatric world, we typically allow at least “one wheeze” before we make any predictions about the future.
Insider Info: Children under 5 years of age who frequently wheeze with colds are often said to have “reactive airway disease” (instead of asthma). Many (but not all) of these kids are diagnosed with asthma down the road, when they’re old enough to undergo asthma testing. The asthma test (spirometry) requires some skill and maturity on the child’s part to get an accurate result (which is why it isn’t usually performed until age 5 or so).
How is Wheezing Managed?
First, the doctor needs to figure out what’s causing the wheezing. If your child swallowed something, then it needs to be removed. If the airways are tightening up because of an infection, medications can be given to reopen them.
2 Types of Medication That Doctors Commonly Use in Acute Wheezing Situations Are:
1. Bronchodilators (such as Albuterol), which dilate the airways.
2. Oral Steroids (such as Prednisolone) which decrease the inflammation in the airways.
Whether the doctor uses these medications depends on the cause of the wheezing and how bad it is.
The Bottom Line
If your child develops a cold, keep an ear out for wheezing and for the barking cough of croup.
Sneak Peek: Next week’s PediaGuide will focus on ear infections and how they’re treated. See you then!

“Ever had a job where you had
no experience, no training,
you weren’t allowed to quit,
and people’s lives were at stake?
THAT’S CALLED PARENTING”



The Reminders for This Week are Essentially the Same as Last Week’s.
- Remember to Give Your Baby a Daily Vitamin D Supplement (That Contains 400 International Units Per Day) If You’re (Exclusively) Breastfeeding OR If They’re Taking Less than 32 Ounces of Formula Per Day.
Get Wise (Again) about the importance of vitamin D supplementation.
- For Formula-Feeding Parents: Make sure you’re mixing the formula correctly and that it has iron in it (which it probably does). Get Wise about How to Mix Formula.
- Put Your Baby on Their Back to Sleep, With No Pillows, Blankets, Bumpers, or Stuffed Animals in the Crib.
- Avoid Giving Honey to Babies Under 1 Year.
Why? Because of the concern for infant botulism. Get Wise about it here.
- Don’t Give Water to Babies Under 6 Months of Age (Except For What’s in the Formula, If Your Baby is Taking Formula).
Why? Because extra water can lead to electrolyte abnormalities (such as low sodium levels), which can, in turn, lead to seizures.
- Call the Doctor If Your Baby Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Don’t Give Ibuprofen to Babies Under 6 Months of Age. Aspirin Is Off Limits For Kids Under 18 Years (Unless It’s Prescribed by the Child’s Doctor).
- Do Tummy Time at Least Twice a Day For a Few Minutes Each Day to Help Strengthen Your Baby’s Neck Muscles and Improve Their Head Control.
And…That’s a Wrap!