Note
This page may contain affiliate links, and I may earn a small commission when you click on them (at no additional cost to you). As an Amazon affiliate, I earn from qualifying purchases. These products were researched and selected with care. However, because things change, make sure to check the safety profiles (and be on the lookout for any recalls) before using them.
Despite what the movies show, breastfeeding can be a challenge and a source of stress for Moms. Moms often feel “like a failure” if the breastfeeding process isn’t easy breezy. Everyone’s experience is different, so treat yourself kindly and know that there’s a learning curve (for both you and your baby) when it comes to breastfeeding. As with learning anything new, learning to breastfeed takes practice and patience. Lucky for you, you’ll be getting a lot of practice breastfeeding because newborns have to feed every 2-3 hours.
Here is Some Basic Breastfeeding Info to Get You Started:
- The first milk that you’ll produce is called colostrum. It’s yellow (sometimes even orange) and is thicker than regular (mature) breast milk. In pediatric circles, colostrum is known as “liquid gold” because it contains nutrients, antibodies, and even a mild laxative to help your baby poop and get rid of the bilirubin (the stuff that causes jaundice – a yellowing of the skin and the whites of the eyes).
- Around Day 3 postpartum, you’ll start producing transitional milk (instead of colostrum), and by the end of the first week of your baby’s life, your milk will become the standard, white breast milk.
- Here’s the Basic Feeding Schedule for the First 2 Weeks of Life:
During the first two weeks (or so) of your baby’s life, you’ll need to feed them every 2-3 hours. That’s 8-12 feedings per day.
Reality Check: Feeding your baby every 2-3 hours (on a set schedule) means that you’ll need to wake them up to feed AND feed them even if they don’t seem all that interested.
In addition to feeding your baby, keep track of their “ins & outs.” This is DocTalk for how much your baby feeds & when (INs) and the number of pees & poops they have (OUTs).
By 2 Weeks of Age, your baby should be back up to their birth weight. As you may remember, all babies naturally lose weight after birth and (ideally) regain it by 2 weeks of age.
From 2-4 Weeks: If your baby is back up to their birth weight at 2 weeks and the feeding is going well, the pediatrician may allow them to feed “on demand” (i.e. when they want to). This will probably mean that you’re feeding your baby every 2-3 hours during the day and every 4 hours (or so) at night.
In addition, the pediatrician may tell you that it’s ok to stop recording your baby’s ins & outs and to merely ballpark them in your head.
- As you get to know your baby, you’ll start to recognize their “hunger cues.” These may include:
- Increased alertness.
- Sucking on their fists.
- Smacking their lips.
- Rooting (turning their head and opening their mouth in search of food).
- Fussiness (in some cases).
Double Take: Not all fussiness means hunger. Crying is a baby’s main mode of communication, so fussiness may just mean that your little one is tired, bored, has a wet diaper or is trying to blow off some steam. Crying tends to be a “late” sign of hunger.
Party Trick:

Pass your baby over to one of your bachelor friends and watch the rooting (i.e. trying to find a nipple) begin. It’s good clean fun for everyone!
Ok. Now That You That Know About Breastfeeding Schedules and Hunger Cues, You May be Wondering How Exactly One Goes About Breastfeeding.
Here are the 3 Main Breastfeeding Steps:
Step 1: Find a Comfortable Position.
In the early days, breastfeeding will probably feel a bit awkward as you try to find a comfortable position and attempt to get your baby to latch onto your nipple. Remember, there’s a steep learning curve for both you and your baby, so be kind to yourself.
The first step is to find a “hold” that feels right to you. There are several options when it comes to breastfeeding positions and it will probably take multiple tries to find the one (or two) that work best for you. Here’s a picture of the most common breastfeeding positions.
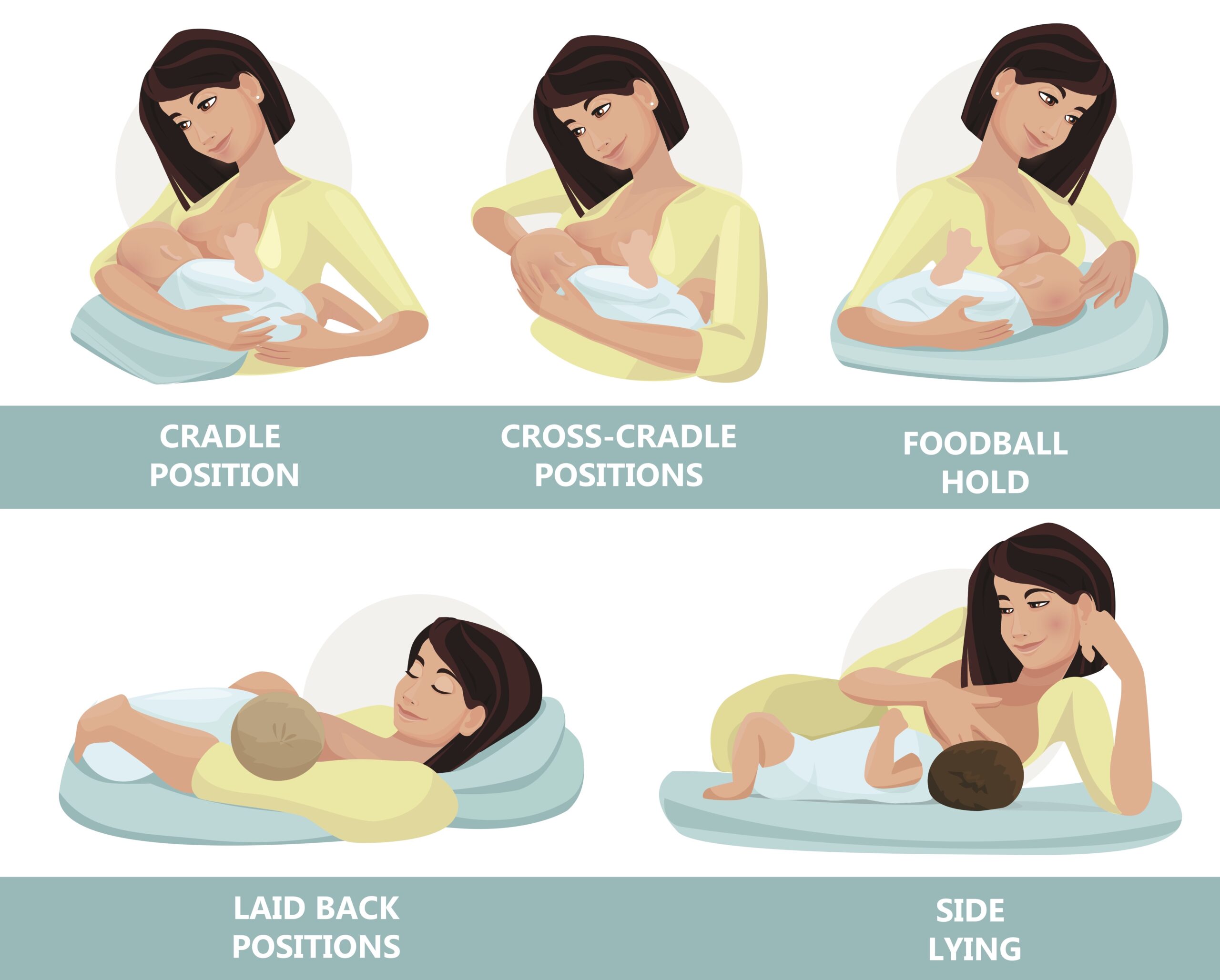
Insider Info:
- Many women start off trying the cradle position or the cross-cradle position (they’re different in terms of which arm is on the bottom) and the football hold. You may end up using different positions, depending on the day.
- Because newborns are tiny, floppy and wiggly, women will often use a nursing pillow, such as the Boppy Pillow or the My Brest Friend Pillow, to better support their little one’s body during the breastfeeding sessions.
- PediaTip: Though tempting, avoid bending over your baby when you feed them. Instead, lean back and lift your baby to your breast (with the support of a breastfeeding pillow). Why? To save your back!
Step 2: After You’ve Picked the Hold That You Want to Go With, Take the Time to Get a “Good Latch.”
The latch is the way that your baby takes your nipple and the surrounding areola (the pigmented skin around your nipple) into their mouth. A proper latch is key and helps prevent sore and bleeding nipples.
You want the latch to be deep enough so that your baby has your entire nipple and areola in their mouth.
Here are 2 Pictures of a Thumbs-Up Latch:
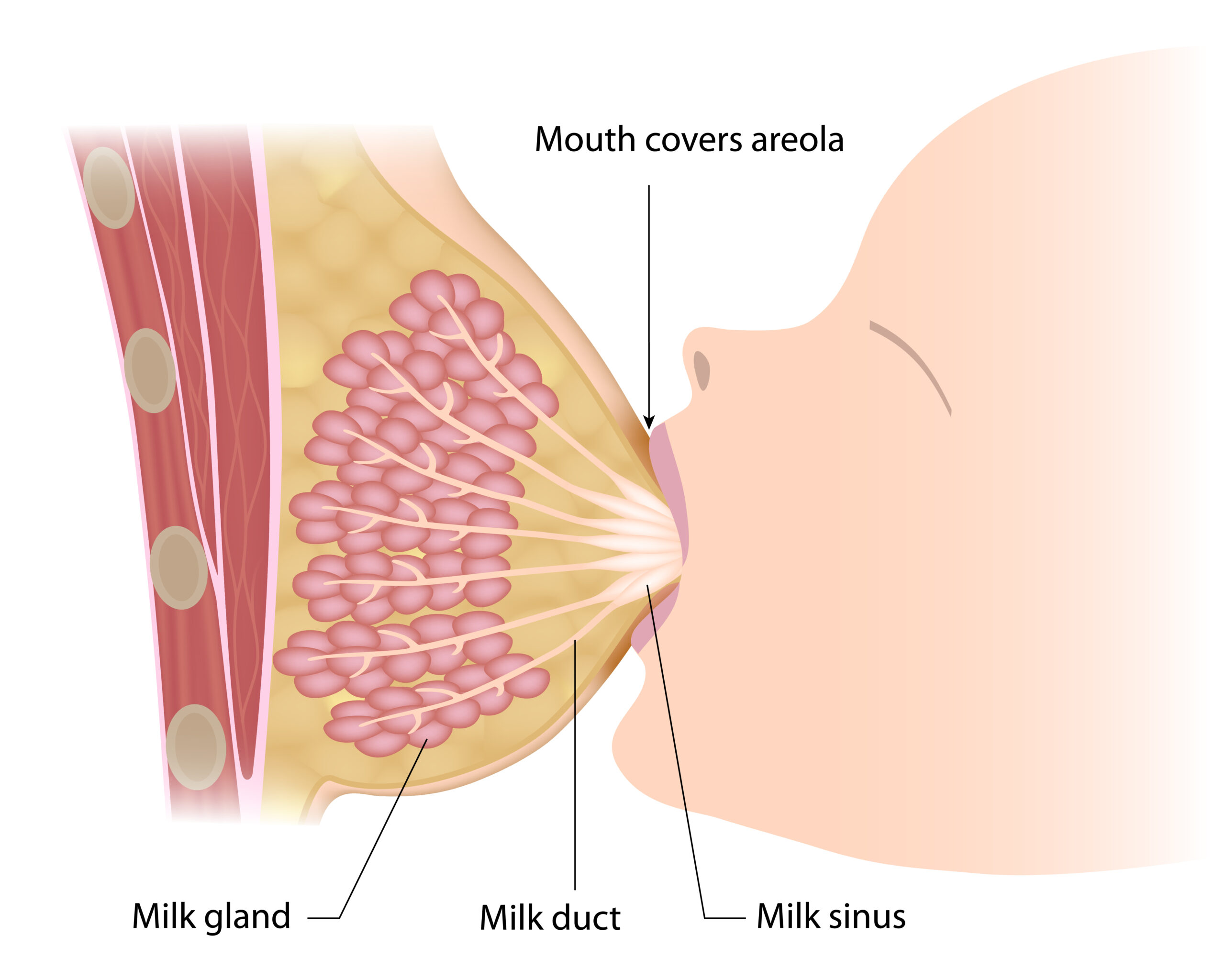

To help your baby get a good latch, pretend that your breast is a sandwich that you want your baby to take a big “bite” out of. To to this, place your thumb above your nipple and your 4 fingers below your nipple (forming a “C” with your hand) and squeeze (softly). This will flatten your breast out and make it easier for your baby to latch onto your nipple. Then, stroke your baby’s nose with your nipple. This will entice them to open their mouth wide. When your baby does open their mouth, (gently) shove your nipple (and your areola) into it.
Insider Info: If you’re using the “cross-cradle” position, hold your breast with your free hand in a vertical “U” position, with your thumb on one side of your nipple and your 4 fingers on the other side. See how the woman in the picture below is using her free hand to gently squeeze her breast?

PediaTip: Avoid the Dreaded Shallow Latch.
A shallow latch is a latch in which your baby only takes the nipple into their mouth and not much (or any of) the areola.
If your baby’s latch is only so-so, detach them from your breast (put your finger in the side of their mouth to break the seal) and try again. After a few days of doing this, your baby will get the memo about what an appropriate latch is.
3. Feed Your Baby for a TOTAL of 20-30 Minutes Per Feed (10-15 Minutes on Each Side). Don’t Be a Hero and Breastfeed for Hours on End.
Why? Because nursing Moms get the most bang for their buck after 20-30 (total) minutes of breastfeeding (i.e. 10-15 minutes per breast). After the initial 20-30 minutes, babies tend to diddle around and use Mom’s nipple as a pacifier (ouch!).
PediaTip: If your baby falls asleep with your nipple in their mouth, you can gently disengage them from your breast and snuggle a bit longer or put them in their crib.
Once your baby gets the hang of nursing, (after a month or so), they’ll become very efficient at it and take only 10-15 minutes total to feed.
Insider Info: Believe it or not, breastfeeding is a workout for babies! For them, it’s like climbing a flight of stairs. That’s why they often conk out after feeding or go into a “milk coma.” Your baby may get sweaty when they breastfeed too. This is usually because of the heat the two of you generate when cuddling skin-to-skin.
Symptom Alert: If your baby gets sweaty during breastfeeding AND they seem out of breath or their lips are turning blue while they feed, let the pediatrician know. Why? Because this can be a sign of an underlying problem (namely of a heart or lung issue). Reality Check: These problems, are rare.
The Bottom Line: Use the tips above to help you get started down the right path on your breastfeeding journey. And remember, learning how to breastfeed can take a little while, so give yourself (and your baby) some time to get the hang of it. If you and your baby are really struggling with breastfeeding, reach out to a lactation consultant (your baby’s pediatrician should be able to recommend one). Some lactation consultants will even come to your house. Score!
Want to Get Even Wiser About Breastfeeding? Check Out the Articles Below From Our Baby PediaGuide! If You’ve Already Purchased the Baby PediaGuide, Simply Click the Links for Instant Access. If You Don’t Have the Baby PediaGuide Yet, You Can Get It in the “Find Your Guide” Section Below…
- The Top 5 Breastfeeding Challenges & Complications. (Think: Mastitis-a Breast Infection- and Flat or Inverted Nipples.)