There are 2 different types of amniocentesis: the “maturity” amniocentesis and the “genetic” amniocentesis. The “maturity” amniocentesis determines how mature a fetus’s lungs are towards the end of pregnancy (in case the baby needs to be delivered early).
The “genetic” amniocentesis, on the other hand, is a prenatal diagnostic test that confirms whether the fetus has a chromosomal abnormality. In this article, we’ll focus on the “genetic” amniocentesis. Get Wiser about it below.
Who Typically Qualifies for a “Genetic” Amniocentesis?
1. Pregnant women 35 years and older.
2. Parents-to-be with a family history of chromosomal abnormalities.
3. Pregnant women whose prenatal screening test results (from the first trimester screen, the second trimester screen, or the NIPS test) fell into the “high risk” category.
When is a “Genetic” Amniocentesis Performed?
Typically between 15-20 weeks of pregnancy.
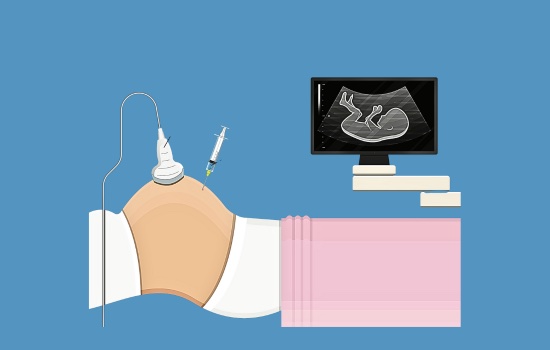
What Happens During the “Genetic” Amniocentesis Procedure?
- A needle is inserted through Mom-to-be’s abdomen under ultrasound guidance to collect a small amount of amniotic fluid from the amniotic sac (the sac the fetus hangs out in). The fluid is then sent to a genetics lab to be analyzed and the results come back in about 10 days.
- The amniocentesis is performed by either a general OB/GYN or by a perinatologist (a high-risk OB/GYN).
- Women must be on bed rest for 24-48 hours after the procedure with restricted activity for 7 days.
Insider Info: Numbing medicine isn’t generally used during the needle insertion, but sources say the pain is tolerable without it.
Unlikely Complications of an Amniocentesis Include (But Aren’t Limited To):
- Bleeding or leakage of amniotic fluid after the procedure.
- Rh sensitization – when mom’s Rh-negative blood (A-, B-, AB-, or O-) starts making antibodies against the fetus’s Rh-positive blood. Fortunately, this complication can be fairly easily prevented by giving Moms-to-be with Rh-negative blood a shot called RhoGAM after the amniocentesis. Get Wise(r) about “Rh incompatibilities” here.
- Needle injury to the baby (this is super unlikely, though, and isn’t usually a big deal if it occurs).
What Will the “Genetic” Amniocentesis Tell Me?
- It will reveal your fetus’s “karyotype” (i.e. their chromosomal make-up) and tell you whether (or not) they have a chromosomal abnormality.
- It will also tell you if your baby has a neural tube defect (a defect of the brain, the spine, and/or the spinal cord).
The Pros of the “Genetic” Amniocentesis:
- The “genetic” amniocentesis is 99% accurate when detecting chromosomal abnormalities.
- It can also reliably diagnose neural tube defects (unlike chorionic villus sampling, another prenatal diagnostic test that’s typically performed between 10-13 weeks of pregnancy).
- In addition, it’s a good option for women who had an abnormal second trimester ultrasound, but aren’t eligible for the chorionic villus sampling (CVS) test because it’s too late in their pregnancy.
- The amniocentesis procedure has a lower rate of miscarriage than the CVS test (but not by much).
This makes the amniocentesis the preferred test for women who want to know if their baby has a genetic problem, but who wouldn’t intervene and terminate the pregnancy if a problem was discovered.
The Cons of the “Genetic” Amniocentesis:
- The genetic amniocentesis is done later in pregnancy (between 15-20 weeks) than the CVS test. This can make things harder in the unlikely event that you have to make a tough decision about whether or not to continue the pregnancy.
Common Question: Will My Insurance Cover My Amniocentesis?

Your amniocentesis should be covered by your insurance if it’s medically indicated. The final answer, however, depends on your insurance provider.
PediaTip: Call your insurance provider prior to the test to make sure the procedure is covered.
The Bottom Line
If your doctor recommends that you undergo prenatal diagnostic testing, ask them if a “genetic” amniocentesis is right for you.