Welcome to Month 34 (Week 1) of Parenting Your Toddler!
In This Week’s PediaGuide Article, We’ll Discuss:
- The Hot Topic for the Week: The 411 on Sinus Infections.
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

A little while ago, I told that sinus infections are rare in babies under 1 year. Now that your child is a toddler and their sinuses are better developed, sinusitis is more of a possibility. Although sinus infections aren’t super common in toddlers, they’re still something to keep on your radar.
One key sign of a sinus infection is a stuffy nose (or a dry cough) that refuses to clear up and may, in fact, be getting worse. Snot that turns green is another red flag (although not all green snot is sinusitis).
Get Wise below about sinusitis and how it’s treated.


Sinus Infections (Fancy Name: Sinusitis)
What is Sinusitis?
Sinusitis is an infection of the sinuses.
Sinus infections occur when fluid (read: snot) sits in the sinuses for too long and gets infected by either bacteria or a virus. For this reason, sinusitis often follows a cold or a runny nose due to allergies.
If a virus infects the fluid, the patient will develop “viral sinusitis.” If bacteria are to blame, they’ll develop “bacterial sinusitis.”
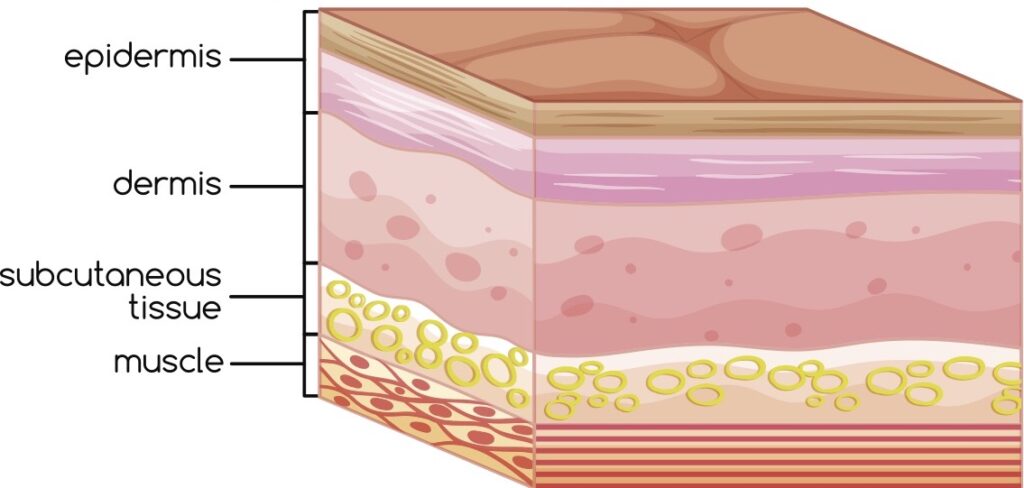
What are Sinuses, Anyway?
Sinuses are the air-filled cavities in our skull & face bones. Here’s a picture of where the different sinuses are located:
Insider Info: A person’s sinuses aren’t fully developed until their late teen years.
- Babies are born with maxillary sinuses (behind their cheeks) and ethmoid sinuses (between their eyes).
- Around 7 years of age, the frontal sinuses (behind the forehead) develop.
- The sphenoid sinuses (behind the nose) don’t fully form until adolescence.
What are the Signs of Sinusitis?
Kids With Sinusitis Tend to Have the Following Symptoms:
- A Cold That Won’t Clear Up.
- A Persistent, Dry Cough That’s Getting Worse. The cough is typically most intense at night.
Insider Info: The runny nose and/or cough must be present for at least 10 days (without signs of improvement) for a diagnosis of sinusitis to be made.
- Clear Snot Becomes Green Snot. This is a soft sign because green snot doesn’t always mean sinusitis.
Why Does Snot “Turn Green,” Anyway? Snot turns green when the infection-fighting cells of the immune system (aka the white blood cells) release a chemical that attacks the germs causing the illness. This chemical turns the snot green. Although green snot can signal a sinus infection, it can also be seen with the common cold.
- A Fever — Especially a High Fever (≥ 102.2ºF for 3+ days) OR a New Fever After Having a “Cold” for Many Days.
Note: High fevers are more commonly associated with bacterial sinusitis than with viral sinusitis.
- Your Child is Cranky, Seems Tired, Has Bad Breath, and Has Circles Under Their Eyes.
- Sneak Peek: When your child gets older (think: 6+ years) they may complain of a headache or facial pain with their sinusitis.
- One trick that doctors use to diagnose sinusitis is to tap the patient’s forehead. If the child complains of pain when the doctor does this, they may have sinusitis.
- Another trick is to have the child lean forward. If the child feels pressure in their sinuses in this position, that’s another red flag for sinusitis.
- One trick that doctors use to diagnose sinusitis is to tap the patient’s forehead. If the child complains of pain when the doctor does this, they may have sinusitis.
Here’s a Common Bacterial Sinusitis Scenario in Kids:
A child has a low-grade fever at the beginning of their cold. The fever goes away, but the nasal congestion and cough continue. Suddenly the child spikes a new, high fever 5-6 days after the first fever. This second fever suggests that a brand-new infection (in this case, bacterial sinusitis) has developed.
Insider Info: The new fever can also be a sign of pneumonia. Therefore, call the doctor if your child experiences any new fevers after having a cold for a while. The doc will want to examine your child to determine the source of the fever.
How is Sinusitis Diagnosed?
Sinusitis is usually a “clinical diagnosis,” meaning it’s based on the child’s symptoms.
As mentioned above, the symptoms of a runny nose and/or cough must be present for at least 10 days (without signs of improvement) for a diagnosis of sinusitis to be made.
If the case is complicated OR the child doesn’t seem to be getting better with treatment, the doctor may order an X-ray or a CT scan of the sinuses to obtain additional info.
PediaTrivia:

When diagnosing a child with (bacterial or viral) sinusitis, doctors take into account how long the symptoms have been present and if they recur. They then use this information to determine which subtype the sinusitis falls into. The 4 different subtypes of sinusitis are:
- Acute Sinusitis: In this case, the symptoms (nasal congestion and/or a cough) last for 10 days to 1 month.
- Subacute Sinusitis: The symptoms are present for 1-3 months.
- Chronic Sinusitis: The symptoms hang around for 3+ months.
- Recurrent Sinusitis: The child has 4 or more episodes of sinusitis in 1 year.
How is Acute Sinusitis Treated?

- Bacterial Sinusitis is treated with antibiotics. A popular treatment regimen for uncomplicated bacterial sinusitis is a 10-day course of Augmentin (fancy name: Amoxicillin-Clavulanate). For more severe cases, a higher dose of Augmentin may be used. If your child has a penicillin allergy and can’t take Augmentin (because it contains Amoxicillin, an antibiotic in the penicillin family), don’t worry, there are other treatment options out there.
- Viral Sinusitis doesn’t respond to antibiotics. In the case of viral sinusitis, supportive care is the way to go. You can give your child Tylenol or Motrin as needed for fevers and encourage them to rest and hydrate. If your kiddo has an underlying seasonal allergy, the doctor may recommend steroid nose drops (to reduce the inflammation), nasal irrigation (to wash the snot out of the nose), and/or a nasal decongestant (to clear up the congestion).
Double Take: It can be hard to tell bacterial sinusitis and viral sinusitis apart. Even though viral sinusitis is more common than bacterial sinusitis, doctors tend to err on the side of caution and put kids on antibiotics if the symptoms have been going on for 10+ days and are interfering with the child’s quality of life.1
A Word About CHRONIC Sinusitis:
If your child develops chronic sinusitis (i.e. sinusitis that lasts more than 3 months despite treatment) OR recurrent sinusitis (multiple bouts of sinusitis), the pediatrician will probably refer them to an allergist or to an ENT (an ear, nose, and throat doctor).
Why? Because these specialists are pros at figuring out whether a never-ending (or always returning) case of sinusitis is due to an allergy or to a structural problem in or around the nose (such as a nasal polyp) that needs to be treated.
The Bottom Line
Although sinusitis isn’t very common in toddlers, it can occur. Call the doctor if your child has a runny nose that persists for 10 (or more) days OR if they spike a new fever 5-6 days after the start of a cold.
“What is a home
without children?
Quiet.”
~Henny Youngman


The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
- Limit Your Child’s Whole Milk to 16-20 Ounces Per Day (Starting at 2 Years of Age).
- Feed Your Child What You Eat, But Cut Into Bite-Sized Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
- Keep Your Child in the Rear-Facing Position in Their Car Seat Until They Exceed the Height and Weight Restrictions Outlined by the Manufacturer.
And…That’s a Wrap!