Welcome to Month 32 (Week 2) of Parenting Your Toddler!
In This Week’s PediaGuide Article, We’ll Discuss:
- The Hot Topic for the Week: Cuts and Stitches.
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

This week, we’ll continue our theme of injuries in toddlers by revisiting the topic of cuts and what to do about them. Get Wise (again) about how to clean cuts and when to get them stitched up. We’ll also review the Top 15 Items to Have in Your First-Aid Kit.


Cuts & Stitches
Most Cuts and Scrapes are Minor and Heal on Their Own.
If Your Child Gets a Cut and It’s Bleeding, Do the Following:
1. “Hold pressure” (with a tissue or a piece of toilet paper) to stop the bleeding.
2. Clean the cut with soap and water.
3. Inspect the cut.
4. After you’ve examined the cut, it becomes a choose your own adventure story based on what the cut looks like:
- Option #1: If the cut is minor, apply an anti-bacterial ointment (such as Neosporin) to the affected area and cover it with a Band-Aid.
Insider Info: Back in the day, doctors recommended “airing out” cuts thinking they healed better and faster when they were left uncovered. Now, studies show that keeping cuts moist and covered is the way to go.1
PediaTip: Check the cut daily to make sure that it’s not getting infected.
- Option #2: If the cut looks worrisome, your child may need stitches. In this case, call the doctor.
Medical Attention is Usually Needed in the Following Situations:
- The Cut is Deep and Gaping. These types of cuts often require stitches.
Insider Info: The depth of a cut can be hard to assess, so err on the side of caution and call the doctor if you’re not sure. If you see globs of fat oozing out of the cut, you know that it’s deep.
- You Can’t Get the Bleeding Under Control Despite Holding Pressure for 10-Plus Minutes.
- The Wound Is in a Tricky Location. Lacerations in the following areas may need to be sutured by a plastic surgeon for cosmetic reasons and to prevent complications.
- Cuts in the upper part of the ear.
- Cuts at the hairline.
- Cuts that run across the eyebrow.
- Cuts in the nasal septum (i.e. in the bone & cartilage that divides the two nostrils).
- Eyelid cuts.
- Cuts through the upper or lower borders of the lip (fancy name: the vermilion borders).
Note: Cuts on the lip itself don’t usually require stitches.
Insider Info: It’s rare to need stitches on the tongue or the gums. Why? Because these areas tend to heal well without stitches (unless the tongue is cut all the way through, which it’s usually not).
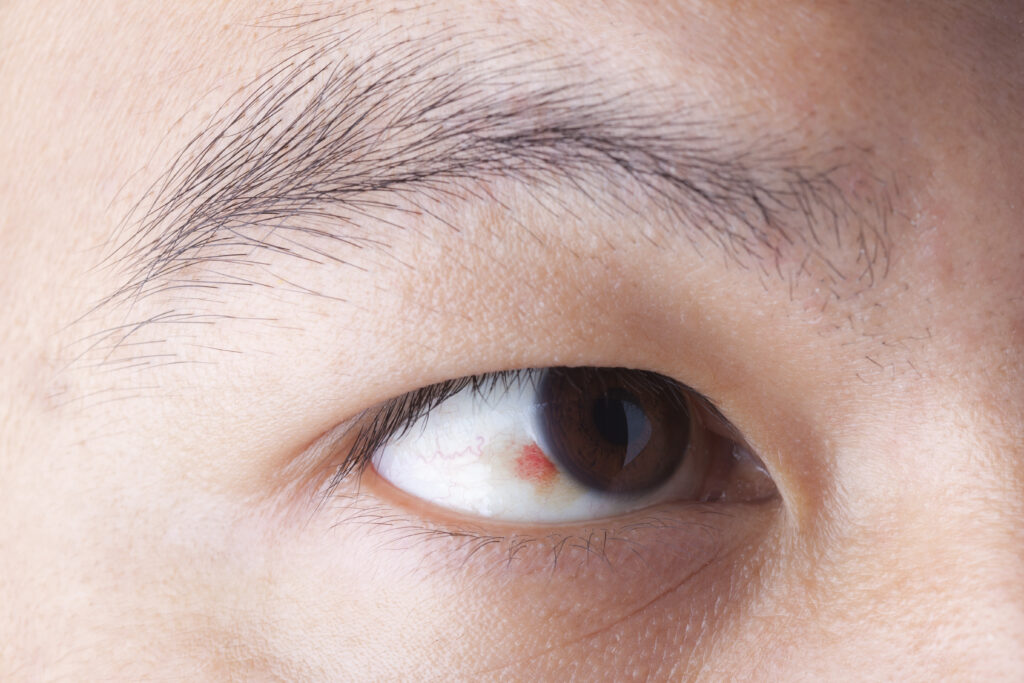
Other Situations That Typically Require Medical Care, Include Those in Which:
- The Wound Starts Getting Infected Over Time (i.e. your child spikes a fever or the cut turns red, starts to ooze pus, or becomes more painful).
- The Cause of the Cut (i.e. the Mechanism of Injury) Makes It More Likely That the Cut is Going to Get Infected (i.e. That it Will Become a “Dirty” Wound). Animal bites, human bites, and cuts from a rusty nail are all considered “dirty” wounds.
- Your Child’s Immunizations Aren’t Up To Date. In this case, your child may need a tetanus booster.
Not Sure If Your Child’s Tetanus Series is Current (or Adequate)? Ask their doctor. Know too, that kids usually get tetanus shots at 2 months, 4 months, 6 months, 15 months, and again at 4 years. They get an additional tetanus booster shot at 11-12 years and a tetanus booster every 10 years after that.- For “clean” wounds, a tetanus booster is recommended if the child has gotten fewer than 3 doses of the tetanus vaccine OR if the most recent tetanus shot was administered 10+ years ago.
- For “dirty” wounds, a tetanus booster is needed if the child has gotten fewer than 3 doses of the tetanus vaccine OR it’s been 5+ years since the last tetanus shot.
PediaTip: If you’re concerned about your child’s cut, don’t wait to seek treatment. Why? Because it’s best to get stitches within 12 hours of injury, ideally within 6-8 hours. After that, the risk of infection goes way up.
If the doctor thinks your child needs stitches based on the clues above, they’ll tell you where to go.
The Options Are: The doctor’s office, a plastic surgeon’s office, the ER, or an urgent-care center (that has doctors well-versed in pediatrics).
Getting Stitches
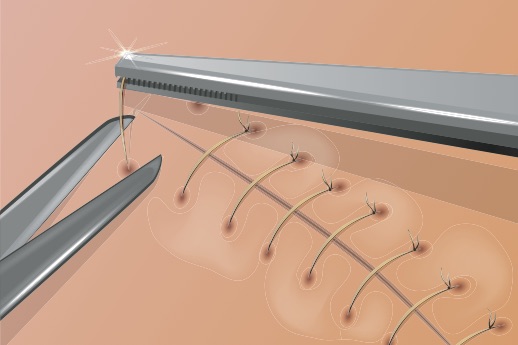
Before stitching a child up, the doctor will clean the wound thoroughly, numb the area with a local anesthetic (such as injectable Lidocaine), then put the stitches in with a medical needle and thread.
As you can imagine, toddlers hate all of this. The biggest challenge will be keeping your child STILL. This is one of the few cases in which bribery gets the thumbs-up. If your child is in total meltdown mode, the doctor may suggest a sedative or an anti-anxiety medication to help calm them down.
FYI: Stitches Aren’t the Only Game in Town.
- Glue (e.g. Dermabond) and Steri-strips (butterfly bandage closures) can be used for small, straightforward cuts.
- Staples are commonly used for cuts on the scalp. Although head wounds tend to bleed a lot, only a few staples are usually needed to close them. Don’t worry, the doctor isn’t pulling out an office stapler for this; a fancy staple gun is used instead. Putting staples in a child’s head may sound kind of barbaric, but they go in fast and do the job well.
Common Questions About Stitches:

Few Kids Escape Childhood Without Needing at Least a Few Stitches. Here are the Top 3 Questions Parents Tend to Ask About Them:
1. Do Stitches Dissolve on Their Own?
Some of them do. Your child’s doctor (or the ER doctor) will tell you what type of suture material they used to repair the cut.
2. When Will the Stitches be Removed?
It depends on the location of the cut and what type of stitch material was used.
If the stitches are dissolvable, they don’t have to be removed (and will dissolve on their own). In this case, you don’t have to do anything except watch for signs of infection.
If the stitches are not dissolvable, then location matters. For example, stitches on the face are typically removed after 5 days, whereas stitches in the leg, are taken out after 8-10 days. Ask the doctor when your child should return to have the stitches removed and who will do it (the general pediatrician or the ER doctor)?
3. Can Stitches Get Wet?
Non-dissolving stitches should be kept dry and covered for the first 48 hours.
Dissolvable stitches must be kept dry longer.
Ask the doctor what they recommend based on your child’s specific case.
Bonus Question: Will My Child Have a Scar?

The answer to this question depends on the severity of the cut, where it is on the body, and how well the stitches are cared for.
Tips for Minimizing Scarring Include:
- Apply sunscreen to the area daily, after the wound has healed. Do this for (at least) the first year after the injury, even during the winter.
- Try a scar-minimizing cream like Mederma, which is sold both online and over the counter at your local drugstore. Get the green light from the doctor before using it, though.
- Follow-up with the doctor as instructed.
Why? Because leaving the stitches in for too long can result in suboptimal healing.
The Bottom Line: Most cuts in kids aren’t serious. That being said, call the doctor (or head to the ER) if you think your child needs stitches.
A Review: The Top 15 Items to Have in Your First-Aid Kit

Cuts, Scrapes, and Falls Are an Inevitable Part of Growing Up. To Help You Prepare for Them, Here are the Top 15 Items to Include in Your First-Aid Kit.
1. Band-Aids (of varying sizes).
2. Elastic Wrap Bandages.
3. Athletic Tape.
4. An Instant Cold Compress (aka an ice pack).
5. Alcohol Wipes (to clean cuts and remove residue from Band-Aids and athletic tape).
6. Hydrogen Peroxide (you can pour hydrogen peroxide on cuts to disinfect them).
7. Eyewash Solution.
8. Vaseline.
9. Neosporin (an anti-bacterial ointment for cuts and scrapes).
10. Calamine Lotion (to help with itchy rashes, like poison ivy).
11. Acetaminophen (e.g. Tylenol) and Ibuprofen (e.g. Motrin and Advil).
12. Benadryl.
Note: Benadryl is typically reserved for children 2 years & older when it’s used for (minor) allergic reactions. When it’s used as a decongestant, Benadryl is often limited to kids 6 years & older (unless the doctor says otherwise). If your child has an Epi-Pen, add it to the kit as well.
13. 1% Hydrocortisone cream (a steroid cream).
14. A Thermometer.
15. Scissors and Tweezers.
The Bottom Line
Call the doctor if your child’s cut or injury requires more than what’s in your first-aid kit.
“Marriage is mostly just sending
each other memes while your kids
destroy the house around you.”
~James Breakwell


The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
- Limit Your Child’s Whole Milk to 16-20 Ounces Per Day (Starting at 2 Years of Age).
- Feed Your Child What You Eat, But Cut Into Bite-Sized Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
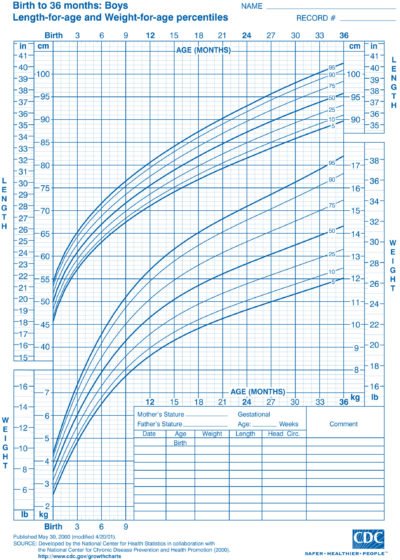
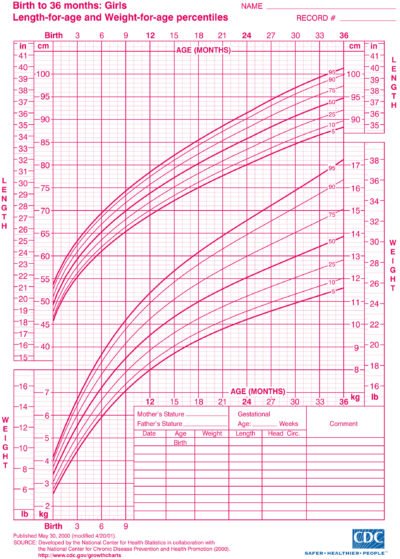
- Keep Your Child in the Rear-Facing Position in Their Car Seat Until They Exceed the Height and Weight Restrictions Outlined by the Manufacturer.
And…That’s a Wrap!