Welcome to Month 29 (Week 1) of Parenting Your Toddler!
In This Week’s PediaGuide Article, We’ll Discuss:
- The Hot Topic for the Week: The 411 on Type 1 and Type 2 Diabetes.
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

As kids get older and discover the glorious world of sweets, parents start to worry about cavities, hyperactivity, and even diabetes. While it’s true that sugar can cause cavities, the link between sugar and hyperactivity & diabetes is less clear.
To Prevent Cavities:
- Brush your child’s teeth twice a day (especially before bed) with a fluoride toothpaste.
Note: At this age, the amount of toothpaste on the toothbrush should be roughly the size of a grain of rice.
- Avoid giving your kiddo juice or milk at night in their crib or toddler bed.
- Have your child drink filtered tap water.
Exception: If your family drinks well water or you have iffy tap water, then you may have to boil the water first or use bottled water.
- Schedule regular visits to the pediatric dentist.
Sugar and Hyperactivity:
When it comes to hyperactivity, researchers say that sugar does not cause ADHD. They even go so far as to say that sugar does not “appear to affect behavior in children.”1 Many experts think the “high” that parents see after their child eats cake at a birthday party is due to their excitement (rather than to sugar). Still, most parents tend to blame the sugar.
And What About Sugar and Diabetes?
There are two types of diabetes seen in children and teens: Type 1 Diabetes and Type 2 Diabetes. In both types of diabetes, patients have trouble regulating their sugar (aka glucose) levels, but neither type is directly caused by sugar consumption. (Obesity is, however, a risk factor for Type 2 diabetes.) That being said, when a person has diabetes, eating too much sugar can overload their system and make the symptoms worse. Although diabetes is rare in young children, it doesn’t hurt to be aware of the red flags signs for it, just in case.
Get Wise About Type 1 and Type 2 Diabetes Below.


The 411 on Type 1 and Type 2 Diabetes
Although the Causes and Treatment of Type 1 and Type 2 Diabetes Differ, the Presenting Symptoms are Pretty Much the Same. They Include:
- Frequent urination. In kids, this may manifest as suddenly wetting the bed despite having been successfully potty-trained.
- Fatigue.
- Unintentional weight loss (i.e. the child loses weight despite having a hearty appetite).
- Excessive thirst.
- Breath that smells sweet and fruity.
Insider Info:
- Type 1 diabetes is the No. 1 type of diabetes in kids. Children with Type 1 diabetes are usually skinny and continue to lose weight despite being hungry. Type 2 diabetics, on the other hand, are usually overweight and often have a telltale skin finding called acanthosis nigricans (a darkening and thickening of the skin at the back of the neck, in the armpits, and around the groin area).
- Type 1 diabetes typically shows up between 4-6 years of age, with a second peak occurring around 10-14 years. It can present earlier though (in toddlers) or later (in adulthood).
- Back in the day, if a child developed diabetes, doctors assumed that it was Type 1 diabetes. But now that we’re in the throes of an “obesity epidemic” in the U.S., Type 2 diabetes is on the rise in kids (namely in those 10 years and older).
If Too Much Sugar Doesn’t Cause Diabetes, What Does?
Although Type 1 and Type 2 diabetes have overlapping symptoms, they’re caused by different things.
What Causes Type 1 Diabetes?
- Type 1 diabetes is an autoimmune disease that attacks the insulin-producing cells of the pancreas. (The pancreas is located in the abdomen, behind the stomach.)
- What is Insulin and Why is it Important? Insulin is a hormone that brings sugar (glucose) into our cells so that it can be used. If our insulin-producing cells are destroyed and we have no insulin, the sugar hangs out in our bloodstream and causes problems.
Insider Info:
- Type 1 diabetes tends to run in families.
- It’s thought that kids with a genetic predisposition for Type 1 diabetes develop the disease when a virus or an environmental toxin comes along and tells the immune system to start destroying the insulin-producing cells of the pancreas.
What Causes Type 2 Diabetes?
- People with Type 2 diabetes have a resistance to insulin (vs. a lack of it).
- This “resistance” to insulin is often caused by obesity.
How is Diabetes Diagnosed?

With a Blood Test. This can be either a fasting blood test or a random blood test. If a patient has one or more of the following, they’re said to have diabetes:
- A fasting blood sugar of 126 mg/dL or more (fasting means there’s been no caloric intake for 8 hours or more).
- A random blood sugar of 200 mg/dL in a patient with symptoms of diabetes.
- A hemoglobin A1C (HbA1c) of 6.5 or more. (This test is most useful for diagnosing Type 2 Diabetes.)
The HbA1c test provides a snapshot of a patient’s (average) blood glucose levels over a 3-month period. For example, an HbA1c of 6.5 or more suggests the glucose levels have been elevated (on average) for the past 3 months. Docs also use the HbA1c test to determine how compliant patients with diabetes have been with their treatment regimens.
How is Diabetes Treated?
- Type 1 Diabetes: Type 1 diabetes is always treated with insulin. Because of this, Type 1 diabetics are considered “insulin dependent,” meaning they need “exogenous” (i.e. outside) sources of insulin (via injections or an insulin pump) to live.
- Type 2 Diabetes: Mild to moderate cases of Type 2 diabetes can often be controlled with a healthy diet and/or oral medications. Severe cases of Type 2 diabetes and ones that fail to respond to oral medications & diet modifications require insulin.
- Type 1 and Type 2 diabetics who take insulin or other glucose-lowering medications must check their blood sugar levels multiple times a day and count how many carbohydrates they eat at each meal. The number of carbohydrates they eat during a meal determines how much insulin they need to “cover the carbs” and bring the glucose into the cells.
Insider Info: Although diabetes is a chronic, life-altering condition, it’s manageable. One of the hardest things about diabetes (especially insulin-dependent diabetes) is that there’s no day off. Kids (with their parent’s help) must be diligent about checking their glucose levels and be careful about what they eat.
What Happens If a Child’s Diabetes Isn’t Well Controlled With Treatment (or Isn’t Treated at All)?
Both Type 1 and Type 2 diabetics can experience acute and chronic complications of their diabetes if it’s left untreated or if their treatment regimen isn’t optimized. Get Wise about these complications below:
1. DKA (Diabetic Ketoacidosis) – An Acute Complication of Diabetes.
- Unfortunately, one of the ways that diabetes (especially Type 1 diabetes) can make itself known in kids is by causing Diabetic Ketoacidosis (DKA). In DKA, the sugar level gets so high that the child becomes acutely ill.
- What Does DKA Look Like? Children with DKA look sick and become dehydrated and lethargic. They tend to breathe deeply and slowly (fancy name: Kussmaul breathing), and their breath develops a fruity, sweet odor. These kids need to be rushed to the ER and then hospitalized afterwards.
- The Good-ish News: ER and intensive care docs are well versed in the management of DKA and almost all pediatricians have treated children with DKA, at one time or another, during their training. There’s even a well-known algorithm that’s used to manage DKA.
Translation: Kids with DKA tend to be in good hands. - The Not So Good News: DKA can be life-threatening and is a tough way for parents to learn about their child’s diabetes diagnosis. Most hospitals have a diabetes educator, though, who can teach parents the basics of how to manage their child’s diabetes once the DKA has resolved.
- The Good-ish News: ER and intensive care docs are well versed in the management of DKA and almost all pediatricians have treated children with DKA, at one time or another, during their training. There’s even a well-known algorithm that’s used to manage DKA.
2. Chronic Complications of Diabetes:
As mentioned above, it’s important for children with diabetes to closely monitor and regulate their blood sugar levels.
Why? Because erratic blood sugar levels can cause long-term problems (in addition to the acute problem of DKA).
Chronic issues seen with diabetes include: kidney disease, vision problems, high blood pressure, nerve damage in the feet & legs, poor growth, and erectile dysfunction (in males, later in life). Children with diabetes are, therefore, closely followed by an endocrinologist (a doctor who specializes in hormones and metabolic disorders). Endocrinologists can help optimize their patients’ treatment plans and help them stay on top of their glucose levels.
The Bottom Line
Although diabetes is rare in toddlers, it’s worth knowing about—especially if there’s a family history of Type 1 diabetes. Be mindful of the red flag signs described above (e.g. fatigue, weight loss, frequent urination, and excessive thirst) and call the doctor if your child consistently experiences one or more of them.
“Booty Call: a shout from the
bathroom letting you know it’s
time to go wipe someone’s butt.”
~@babyhellfire


The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
- Limit Your Child’s Whole Milk to 16-20 Ounces Per Day (Starting at 2 Years of Age).
- Feed Your Child What You Eat, But Cut into Bite-Sized Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
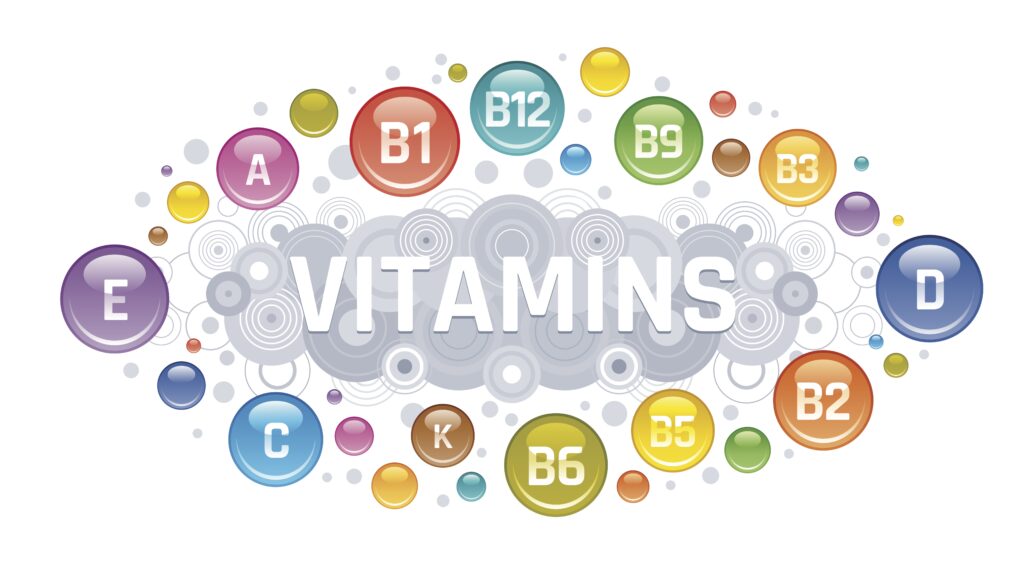
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
- Keep Your Child in the Rear-Facing Position in Their Car Seat Until They Exceed the Height and Weight Restrictions Outlined by the Manufacturer.
And…That’s a Wrap!