Welcome to Month 26 (Week 1) of Parenting Your Toddler!
In This Week’s PediaGuide Article, We’ll Discuss:
- The Hot Topics for the Week, Including:
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

Toddlers can get into habits that are hard to break, such as sucking their thumbs and biting their fingernails. While these habits are not as bad as others (like the habit of ripping off a poop-filled diaper and flinging it across the room), they can increase the transmission of germs and lead to the ingestion of certain parasites (such as pinworms). Thumb-sucking can also lead to dental problems if it goes on for too long.
Learn how to reduce fingernail biting (a new topic) and thumb-sucking (a repeat topic) in the Hot Topics section below. In addition, Get Wise about Pinworm infections and how nail biting and thumb-sucking can cause them.


Pinworm Infections
Pinworms Sound Gross. What are They?
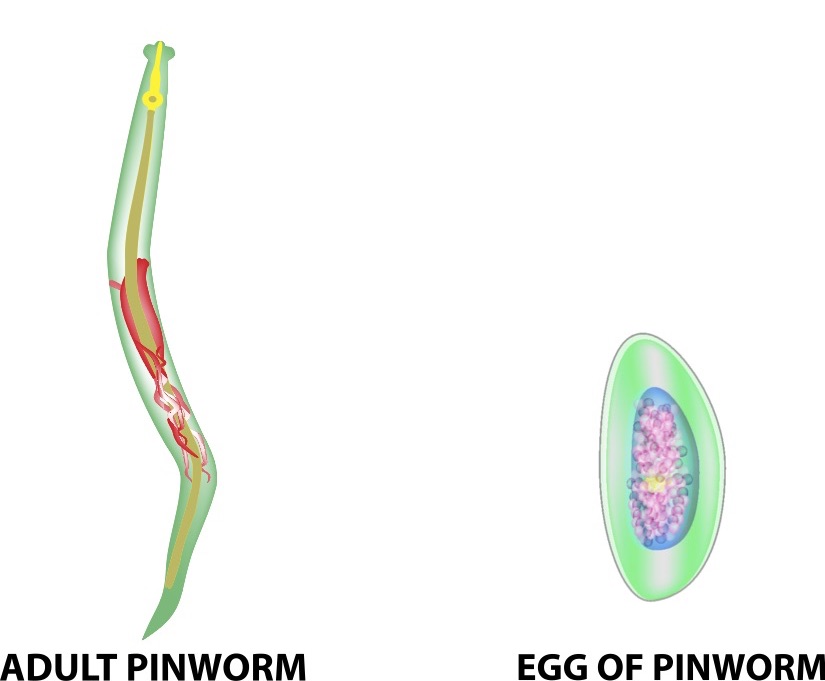
Pinworms (fancy name: Enterobius vermicularis) are small parasitic worms that set up shop in our intestines. Per the Centers for Disease Control and Prevention (the CDC), they’re the most common type of worm infection in the U.S.1
How Do Kids Get Pinworms?
By unintentionally swallowing their eggs.
Uh, Come Again? Yup, when kids swallow the pinworm eggs, the eggs hatch in their intestines. The larvae then grow into mature pinworms in the gut. At night, the mature female pinworms crawl out of the intestines through the anus and lay more eggs.
Yikes. How are the Eggs Ingested?
- The eggs are ingested when kids touch a surface with eggs on them and put their fingers in their mouths.
- Because toddlers and school-aged children like to chew on their fingernails and suck on their fingers, they’re at the highest risk of getting pinworms (although pinworms can be seen in adults too-think: parents and teachers).
Insider Info:
- Pinworm eggs are pretty hearty and can survive on surfaces for up to 3 weeks.
- Sandboxes are a popular pinworm hangout.
What are the Signs That a Child Has Pinworms?
- An Itchy Bum: Your child will have an itchy anus, especially at night.
Why at Night? Because that’s when the females lay their eggs in an itchy mucus-like substance around the anus. Ugh!
- Vaginal Itching (in Girls).
- Loss of Appetite.
- Fussiness.
- Trouble Sleeping.
- Intermittent Abdominal Pain.
How are Pinworms Diagnosed?

If your child is constantly scratching their hiney and having trouble sleeping because of the discomfort, the doctor will suspect pinworms.
To confirm the diagnosis, the doctor will probably do a “scotch tape test.”
How Does That Work? For the scotch tape test, the doctor will ask you to take a piece of scotch tape and stick it to the skin around your child’s anus before they go to sleep (or first thing in the morning before bathing).
If your child has pinworms, the eggs will stick to the scotch tape. The doctor will ask you to bring the scotch tape sample to the office, so they can examine it under a microscope to see if there are any pinworm eggs attached to it.
Insider Info:
- Pinworm eggs are microscopic, meaning you can’t see them without a microscope.
- The worm itself, however, can be seen with the naked eye (it’s tiny, though!). You may, therefore, see the worms in your child’s underwear or stool.
Note: The worms look like tiny pieces of white thread in kids’ poop. Ugh! I know, sorry!
How are Pinworms Treated?

The Good News Is That Pinworms are Fairly Easy to Treat. Here’s How They’re Usually Managed:
- The Doctor Will Recommend That Your Child Take a Medication to Get Rid of the Pinworms.
- A common pinworm treatment for children 2 years and older is Reese’s Pinworm Medicine, a liquid medication.
- Reese’s Pinworm Medicine contains pyrantel pamoate and is available over the counter—no prescription needed.
- Your child will most likely be asked to take one dose of the medication at the time of the diagnosis and another dose 2 weeks later.
Insider Info: ALL family members, regardless of age, should be treated as well.
- In Addition, the Doctor Will Ask You to Take the Following Precautions to Stop the Pinworms in Their Tracks:
- Wash all bed linens in hot water.
- Avoid shaking things that might have eggs on them (such as pajamas, bed linens, and towels).
- Don’t eat in the bedroom.
- Cut and trim the fingernails of all family members. Try to discourage your child from sucking on their fingers or biting their fingernails.
Get Wise re: tips for how to do this below. - Have all family members wash their hands frequently, especially after going to the bathroom and before eating.
- Bathe or shower regularly.
- Don’t share towels.
The Bottom Line: Pinworm infections are pretty common in kids and are, fortunately, fairly easy to treat. If you notice that your child is constantly scratching their bum and having trouble sleeping because of the discomfort, call their doctor.
And Now For a Word or Two About How to Break the Thumb-Sucking and Nail-Biting Habits (to Help Prevent Pinworms).
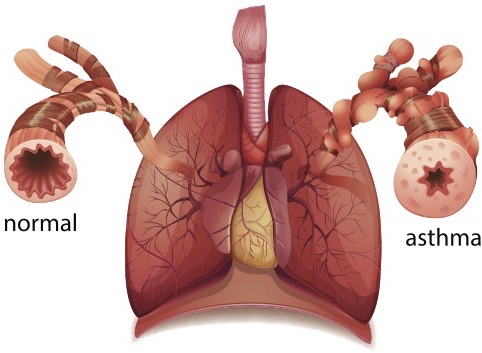
Thumb-Sucking

Thumb-sucking is a common (and normal) self-soothing technique used by babies and toddlers.
The beauty of the thumb is that it’s always with your child and acts as an instant self-soothing tool.
The problem with the thumb is the same: it’s always with your child, making the thumb-sucking habit tough to break.
The Good News?
You have time. Encourage your child leave the thumb-sucking habit in the dust by age 4.
Why?
Because after 4 years of age, there’s a higher risk of dental issues.
Tips for Phasing Out Thumb-Sucking:

- The first step is to set boundaries around the thumb-sucking. For example, tell your child that thumb-sucking is reserved for inside the home (vs. outside of it).
- Avoid the nasty-tasting sprays and constricting thumb splints — they don’t help much. Instead, offer your child a different self-soothing tool (such a blankie or a teddy bear) when they start to suck their thumb.
- Give rewards (for example, a sticker each day) for not thumb-sucking.
- If all else fails, your child’s dentist may be able to hook your child up with a temporary device that attaches to their teeth and prevents the thumb-sucking.
The Bottom Line: If thumb-sucking is your child’s chosen vice, take steps to limit the behavior and to fully extinguish it by age 4.
Nail Biting

Nail biting is a stress reliever for kids and adults alike. As with thumb-sucking, there’s a compulsive element to nail biting. Calling too much attention to this habit can make it worse. The key is to teach your child to reduce the compulsive urge to bite their nails.
Tips for Doing This Include:
- Offering a substitute such as a stress ball or a squishy.
- Encouraging your child to count to 10 before biting their nails.
- Restricting when and where your child can bite their nails (i.e. limiting the nail-biting to their room).
- Taking your child to have a manicure.
- Applying a bitter nail polish to your child’s fingernails as a deterrent. This works better for nail biting than for thumb-sucking.
The Bottom Line
Nail biting and thumb-sucking are common toddler habits that can, in some cases, contribute to pinworm infections. Thumb-sucking can also lead to dental problems if it goes on for too long. Use the tips above to curb these habits and call the doctor if your child develops an itchy bum (especially if it’s worse at night).
“They say women speak 20,000 words a day.
I have a daughter who gets that done by breakfast.”
~Country Living


The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
- Limit Your Child’s Whole Milk to 16-20 Ounces Per Day (Starting at 2 Years of Age).
- Feed Your Child What You Eat, But Cut Into Bite-Sized Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
- Keep Your Child in the Rear-Facing Position in Their Car Seat Until They Exceed the Height and Weight Restrictions Outlined by the Manufacturer.
And…That’s a Wrap!