Welcome to Month 22 (Week 1) of Parenting Your Toddler!
In This Week’s PediaGuide, We’ll Discuss:
- The Hot Topic for the Week: Teaching Toddlers About Personal Space.
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

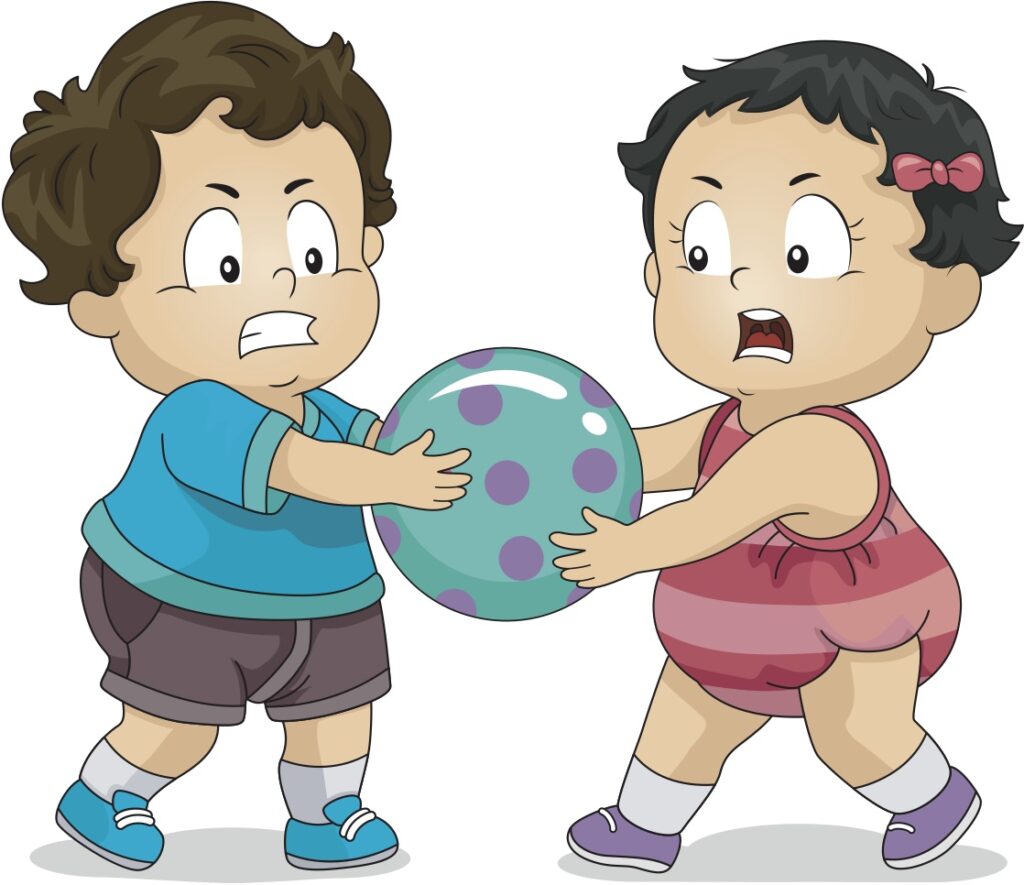
Toddlers, as you probably know by now, are all over the place. They’re often careening from one side of the room to the other and bumping into things. Parents of toddlers are well versed in being hugged too tightly, accidentally elbowed in the face, and stepped on by tiny feet.
When it comes to personal space, toddlers have none and don’t really care about yours either. Although this is developmentally normal, parents often wonder if their child will have poor boundaries with people outside of their family (think: teachers, coaches, and strangers) and will fail to understand when their own boundaries have been crossed.
Although it’s a bit early to talk to your child about “stranger danger” (a term that’s fallen out of favor anyway because strangers aren’t the only ones who can be dangerous), it doesn’t hurt to float the idea of personal space early on.
Get Wise below about how to talk to your toddler about personal space.


Personal Space

If you start lecturing your toddler about “personal space,” they’ll probably have no idea what you’re talking about. The trick is to bring the topic up in a simple and non-threatening way. The best way to do this is to use terms that your child can understand and to read them books about the subject.
Here are 5 Tips to Help You Teach Your Child About Personal Space & Setting Boundaries:

1. Introduce the Concept of the “Body Bubble.”
The body bubble (or the personal space bubble) is a term that’s used to help kids visualize their personal space. Have your child spin around with their arms outstretched and explain that the space within the imaginary circle is their own personal “body bubble.” If your child needs a more concrete visual, you can have them step inside of a hula hoop or stand on a large bathmat.
Once your child gets used to the “body bubble” idea, you can play a game in which they give you a thumbs UP or a thumbs DOWN when you ask to enter their “bubble.”
Reality Check: Body Bubbles can be a difficult concept for toddlers to understand. Don’t worry. The goal is to slowly introduce the language of personal space over time, so that your child eventually gets the hang of it.
2. Remember That Body Bubbles Are Dynamic.
As we all know, body bubbles fluctuate in size based on our moods, our surroundings, and the people with whom we’re interacting.
Sometimes we want to be cozy and other times we need our space. Encourage your child to honor their changing body bubble size by asking if they want a hug rather than assuming so. While asking for permission for affection may feel a bit stilted in the beginning (and definitely doesn’t have to happen all of the time), it’s a helpful habit to get into when you’re teaching your child about personal space.
3. Don’t Force Intimacy.

Although it can be a tad embarrassing when your child hides (or screams) when an out-of-town relative comes to visit, resist the urge to force your little one to hug, kiss, or go towards people they’re skeptical of in the moment.
To make things a little less awkward, you can teach your child different (yet polite) ways to greet someone. In my daughter’s elementary school, they encouraged kids to greet the teachers with an “H, H, or H” — a hug, a handshake (knuckles work, too), or a high-five.
I would throw in two non-touching options as well: simply saying “hi” or waving. By offering your child different ways to greet people, you’re teaching them to honor their inner voice while still being courteous.
4. Talk About Your Own Personal Space.
Work the idea of body bubbles into your daily conversation. For example, invite your toddler into your “body bubble” to snuggle and note when other people enter your body bubble unannounced by saying something like “Whoa! That woman stepped right into my body bubble.”
5. Join the (Book) Club!

Books are a great way for parents to get their point across without lecturing. Although I haven’t found many books about personal space that are specifically geared towards toddlers, there are a few books for kids 4-8 years that can be tailored to fit younger children’s needs. To make these books developmentally appropriate for your toddler, show them the pictures and add your own narrative.
These Books Include:
- “Harrison P. Spader, Personal Space Invader,” by Christianne C. Jones.
- “Personal Space Camp,” by Julia Cook.
- “Hands Off, Harry,” by Rosemary Wells.
Sneak Peek:
Older kids may benefit from the following books, as well:
- “The Berenstain Bears Learn About Strangers,” by Stan and Jan Berenstain.
- “No Trespassing — This Is My Body,” by Pattie Fitzgerald.
The Bottom Line
Over time, your child will learn to set boundaries and develop a sense of their personal space. Introduce the language early on but don’t expect your toddler to always respect your personal space or to be aware of their own. These concepts can take a while to understand and internalize.
Celebrities are Just Like Us!
I’d walk through fire for my daughter.
Well not FIRE, because it’s dangerous.
But a super humid room.
But not too humid,
because my hair.”
~Ryan Reynolds


The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
- Limit Your Child’s Whole Milk to 16-24 Ounces Per Day.
- Feed Your Child What You Eat, But Cut into Small Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
- Keep Your Child in a Rear-Facing Car Seat Until (At Least) 2 Years of Age.
And…That’s a Wrap!