Welcome to Month 19 (Week 1) of Parenting Your Toddler!
In This Week’s PediaGuide, We’ll Discuss:
- The Hot Topic for the Week: Abdominal Pain in Toddlers. Sub-Topics Include:
- Plus, a Few Friendly Reminders.
Get Wise About It All Below…

At 19 months, your child continues to hone their motor skills, language skills, and social skills. Your toddler is probably walking at this point, even running, and climbing the stairs one at a time. Your little one may also have 6-10 words in their vocabulary (in addition to Mama & Dada).
Around 2 years of age, your child will start to put 2 words together to form a rudimentary sentence (such as “That mine” or “No, mine”).
Insider Info: As kids near the 24-month mark, the word “mine” becomes almost as popular as the word “no.”
This week’s PediaGuide article focuses on abdominal pain in toddlers. A wide variety of things can cause abdominal pain in this age group, from good old constipation to more worrisome (and rarer) ailments like appendicitis.
Get Wise below about what doctors worry about when it comes to abdominal pain in toddlers and the questions they ask to determine what’s causing it.


Abdominal Pain in Toddlers
Abdominal pain in toddlers is typically caused by gas, heartburn (reflux), constipation, or a GI virus. Although most abdominal pain is benign and self-limiting, doctors are always on high alert for a “surgical” abdomen. What’s That? As the name implies, a “surgical” abdomen is a gastrointestinal problem that requires immediate attention and (usually) surgery. Examples of a surgical abdomen include:
- Appendicitis – an infection of the appendix that leads to “right lower quadrant pain” – i.e. pain in the right lower side of the abdomen. Get Wise(r) about appendicitis below.
- A Bowel Obstruction – such as a blocked intestine due to Meckel’s diverticulum (an abnormal “outpouching” of the lower part of the small intestine).
- Intussusception – when one part of the intestine telescopes into another part.
- A Strangulated Inguinal Hernia or Umbilical Hernia. “Strangulated” means the blood supply to the hernia has been cut off.
Insider Info: Not all abdominal pain originates in the GI tract. Conditions such as pneumonia, kidney infections, bladder infections, abdominal migraines (i.e. migraines that manifest as stomach pain), and strep throat can cause abdominal pain, as well.
The Top 10 Questions Doctors Ask About Abdominal Pain

Doctors Want to Know the Following Info When They’re Evaluating Abdominal Pain and are Trying to Rule Out a Surgical Abdomen:
1. Is the Pain Acute or Chronic?
Did the pain come on suddenly or has it been going on for a while? When did it start and what was your child doing when it started?
2. Is the Pain Severe (ER-Worthy)?
Fortunately, most abdominal pain doesn’t require a trip to the ER. That being said, here are a few pain-related symptoms that do require a call to the doctor and (typically) a visit to the ER:
- Your child looks sick and isn’t interested in eating or playing with their favorite toys.
- Your kiddo is crying because the pain is so intense.
- The pain seems to be getting worse and is showing no signs of letting up (e.g. it’s been bad for 2+ hours).
- Your child refuses to walk because of the pain.
3. Where’s the Pain?

The Location of the Abdominal Pain Can Provide Clues About What’s Causing It.
- Unfortunately, younger children (under 3 years) are notoriously unreliable when it comes to identifying the location of their belly pain. Toddlers will usually just point to the middle of their abdomen when asked where it hurts.
- Older kiddos are better at pinpointing their pain.
PediaTip: Your child may be better able to localize their pain if you push on different parts of their abdomen. For example, they may wince or say “Ow” when you press on a tender area.
Doctors Divide the Abdomen Into 4 Sections (aka Quadrants) When Describing a Patient’s Pain:
Here’s a Quick Anatomy Lesson to Help You Make Sense of These Quadrants and What They Contain:
- The Left Upper Quadrant: The left upper quadrant houses the stomach and spleen.
- The Left Lower Quadrant: The left lower quadrant contains part of the colon.
- The Right Upper Quadrant: The liver and gallbladder live in the right upper quadrant.
- The Right Lower Quadrant: The appendix and the upper part of the colon are located in the right lower quadrant.
4. Does Anything Make the Pain Better or Worse?
Does the pain change when your child eats, has a bowel movement, or takes medicine? What about when they move around or lie down in a certain position (such as on their back)?
5. Is the Pain Constant or Does it Come and Go?
In the medical world, abdominal pain that “comes and go” is described as “colicky.”
6. Are There Any Other Symptoms Besides the Abdominal Pain?
Examples of additional symptoms include vomiting, diarrhea, blood in the poop, pain with urination, a poor appetite, a sore throat, a rash, a cough, and a runny nose.
7. When Was the Last Time Your Child Pooped? Was the Stool Hard or Soft?
Constipation and gas can cause pretty significant abdominal pain in kids (and in adults too). Therefore, it’s not uncommon for parents to rush their child to the ER worried about appendicitis and sheepishly return home with a diagnosis of constipation.
8. Has There Been Any Exposure to Animals?
In this case, doctors are looking for possible parasites in the gastrointestinal tract.
9. Have There Been Any Recent Stressors at Home or at School/Daycare?
Anxiety and depression can manifest as physical symptoms (such as stomach pain or fatigue).
Insider Info: Doctors will often ask school-aged children if their abdominal pain is present on the weekends, too.
Why? Because kids who have anxiety about going to school may say their stomach hurts during the week, but not on the weekend.
10. Have There Been Any “Sick Contacts?”
This is the fancy way of asking whether a child has been around anyone with similar symptoms (e.g. at home or at daycare).
When the Doctor Examines the Patient, They’ll Be On the Lookout for the Following Red-Flag SIGNS:

- A child with abdominal pain who looks sick (not just nauseated).
- Abdominal pain that starts in the middle of the abdomen, then localizes to the right lower quadrant (docs worry about appendicitis in this case).
- Vomiting bile (green stuff).
- Lethargy.
- Poor feeding and dehydration.
- Bloody poop.
- A tense, bulging belly.
- Abdominal pain that won’t go away.
- A high fever (think: 102.2ºF and above for this age group).
- A child who refuses to walk or play because of their abdominal pain.
Plus, Anything Else the Parents are Worried About!
A Word About Gastrointestinal Ulcers

Peptic ulcers, which include ulcers in the stomach (fancy name: gastric ulcers) and ulcers in the first part of the small intestine (fancy name: duodenal ulcers) can also cause abdominal pain in children. Although peptic ulcers aren’t very common in kids, they’re something doctors think about, especially when the abdominal pain is chronic.
A bacterium called Helicobacter pylori (more commonly known as H. pylori) is the No. 1 cause of peptic ulcers. Doctors can check their patients for H. pylori with a blood test, stool study, or “breath test.”
A GI doctor may also want to confirm the presence of the ulcer with an upper endoscopy. This procedure requires sedation and involves putting a tube with a camera on the end of it down the child’s throat to visualize the stomach and small intestine.
Ulcers caused by H. pylori can be treated with a combo of antibiotics and antacids.
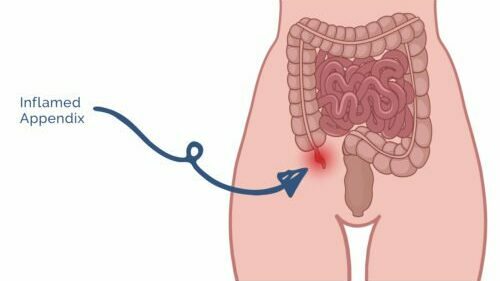
The 411 on Appendicitis
Appendicitis is the No. 1 cause of emergency abdominal surgery in children (although it’s not commonly seen in kids under 5).1
What is Appendicitis? It’s when a person’s appendix becomes inflamed or infected.
Quick Anatomy Lesson: The appendix is a finger-like pouch that projects out from the colon. It’s generally thought to be a “vestigial” organ, meaning it doesn’t serve a purpose but is evidence of our evolution. However, some researchers think the appendix may actually be useful and help protect the “good bacteria” in our gut.2
PediaTrivia:

Other vestigial body parts include tailbones, male nipples (sorry, guys!), and wisdom teeth. In addition, goosebumps are considered a vestigial reflex.3
What are the Symptoms of Appendicitis?
The Following Symptoms are Suggestive of Appendicitis:
- Abdominal Pain. Appendicitis pain starts around the belly-button area (fancy name: the periumbilical region), then migrates to the right lower quadrant a few hours later.
- Appendicitis pain hurts!
- If your child tenses up when you press on their abdomen or refuses to walk because it hurts so much, they may have appendicitis.
- A Poor Appetite.
- A Fever.
- Vomiting.
- Irritability.
Insider Info: The symptoms of early appendicitis are often vague, but as the disease progresses, they get worse and more obvious.
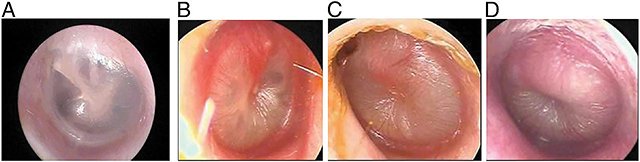
How is Appendicitis Diagnosed?

Appendicitis can be tricky to diagnose, especially in younger kids who can’t verbalize what they’re feeling. If a doctor suspects that a child has appendicitis, they’ll send the child to the ER for lab work and imaging (an abdominal ultrasound or a CT scan).
In young, thin children, an abdominal ultrasound may be all that’s required to make the diagnosis. If the appendix can’t be visualized on the ultrasound, then an abdominal CT scan is needed.
How is Appendicitis Treated?
Appendicitis can be cured by taking the appendix out. Although an “appendectomy” is a major surgery, general surgeons are well-versed in this procedure and can usually do it laparoscopically (without opening the patient up). One of the benefits of laparoscopic surgery is that the scars are barely visible once healed.
Insider Info: Recent studies suggest that uncomplicated cases of appendicitis in older patients may be managed with antibiotics and IV fluids rather than surgery.4 This is not the norm, though, and more research is needed—especially in kids.
PediaWise Book Club

If you’re ever looking for a classic read about a child with appendicitis, check out the first book of the popular children’s book series, “Madeline.” In this book, the star character, Madeline, comes down with appendicitis and goes to the hospital to have her appendix removed. After seeing her enviable scar and all the gifts she receives for being in the hospital, Madeline’s “frenemies” burst into jealous tears, wishing they could have their appendices out too!
The Bottom Line
Abdominal pain is a common pediatric complaint. Fortunately, most cases of abdominal pain aren’t due to a serious medical problem. Call the doctor, though, if you’re worried about your child’s abdominal pain or if they develop any of the red flag symptoms above.
“My friend asked me recently
what the most difficult
part of being a parent is.
‘Without a shadow of a doubt,
it’s the kids,’ I replied.”
~Baby Berry


The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
- Limit Your Child’s Whole Milk to 16-24 Ounces Per Day.
- Feed Your Child What You Eat, But Cut into Small Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
- Keep Your Child in a Rear-Facing Car Seat Until (At Least) 2 Years of Age.
And…That’s a Wrap!