Welcome to Month 15 (Week 4) of Parenting Your Toddler!
In This Week’s PediaGuide, We’ll Discuss:
- The Hot Topic for The Week: Injuries in Toddlers and How to Manage Them. This Hot Topic is chock-full of info, so read it at your leisure OR simply pick & choose the subjects that interest you the most. Specifically, we’ll talk about:
Get Wise About It All Below…
Unless your child is living in a bubble, they’re going to get some bumps and bruises along the way. As toddlers explore, they often run into things, fall down, then get back up and do it all over again.
In theory, we want our children to take risks and develop grit and resilience. In reality, it can be hard to watch. Know that some of these bumps and bruises will happen no matter how much you hover. What you want to guard against are the high-risk injuries — for example, running into traffic, falling down a marble flight of stairs, and catapulting from a dangerous height. Prioritize preventing these types of injuries and do your best with the rest.
The Hot Topic for this week focuses on injuries, including ones that lead to bruises, leg pain, cuts, and splinters. We’ll also provide tips on how to stock your first-aid kit. Get Wise about these topics below.
Bruises
Most bruises in kids are normal and are nothing to worry about. Kids are always bumping into things and taking tumbles, so we expect a certain amount of bruising, especially in “high trauma” areas like the forehead, shins, knees, and elbows.
What Docs Worry About: In rare cases, bruising can be caused by a low platelet count (which leads to blood-clotting issues) or another bleeding disorder. Doctors also worry about “non-accidental trauma” (the PC word for child abuse) in certain situations.
Red Flags: The Following Signs Tend to Get the Doctor’s Attention When it Comes to Bruising:
1. Bruising in Non-High-Trauma Areas (Such as on the Ears, the Neck, and the Cheeks).
2. A Ton of Bruising in Various Places (More Than Normal).
Insider Info: It can be hard to tell what a “normal amount” of bruising is, so ask your child’s doctor what they think.
3. Nosebleeds and Bleeding Gums in Addition to the Bruising. This may be a coincidence or indicate an underlying bleeding disorder.
4. Petechiae – small round pink or purple dots (see pic below).
Why Do Doctors Care About Petechiae? Because they signify bleeding under the skin.
Here’s a Clue That the Dots are Petechiae: Petechiae don’t blanche (i.e. turn white when you press on them).
5. Bruising in a Child With a Family History of a Bleeding Disorder (Such as Hemophilia).
6. Bruising in an Infant Who’s Not Yet Mobile (This Can Be a Sign of Non-Accidental Trauma).
7. Any Bruising That You Find Worrisome.
Why? Because it never hurts to be on the safe side.
The Bottom Line: Call the doctor if you see any of the red flag signs above.
Finger & Toe Injuries
Below are a few classic finger and toe injuries seen in toddlers.
Slammed Fingers
Slammed fingers are common in kids.
Here’s a Classic “Slammed Finger” Scenario: A parent accidentally slams their child’s finger in a car door. The child screams bloody murder and the parent wants to crawl under a rock.
The Management? Years of guilt and therapy for the parent (JK!) and ice for the injured finger.
Signs That a Doctor May Need to Get Involved Include:
- The finger is bruised and excessively swollen. In this case, an X-ray may be needed.
Note: It’s a good sign if the child can wiggle their injured finger.
- There’s a cut that may need stitches. In this case, the parent can clean the cut, then call the doctor.
The Bottom Line: Most injuries caused by slammed fingers don’t require a trip to the doctor. Call the doctor, however, if you have any concerns.
A Blood Blister Under the Fingernail (Fancy Name: Subungual Hematoma)
Subungual hematomas can result from accidental finger slamming too. Subungual hematomas occur when blood pools under the fingernail. A doctor may need to drain the blood blister to relieve the pressure.
Broken Fingers & Toes
Broken fingers often require splinting (rather than casting), whereas broken toes are often “buddy taped” (i.e. taped together).
A child with a broken toe may have to wear a boot as well. Why? To prevent them from putting too much pressure on the toe.
Insider Info: Stubbing a toe is a fairly common way for a child to break their toe. Who Knew? So if your child continues to fuss about their toe a day or two after stubbing it, don’t assume they’re being overly dramatic (like I did with my son — eek!).
Leg Injuries After a Fall
Toddlers fall a lot. This is a normal part of life and a sign that they’re curious and practicing new skills. Fortunately, most falls don’t result in an injury (although they can cause a few crocodile tears).
Below are Some Red Flags to Watch Out For If Your Child Falls and Appears to Have a Leg Injury:
- Your Child Refuses to Stand or Walk After the Initial Shock Has Worn Off.
After a fall, kids will often cry and refuse to bear weight on the affected leg. However, once they’ve settled down and gotten distracted by something else, they usually forget about the fall. If your child continues to resist standing or walking despite your attempts to divert their attention, call the doctor.
- Your Child Continues to Be Inconsolable. Crying hysterically after a fall is not uncommon and is usually a reaction to the pain and the surprise of the fall. Once the shock wears off and the pain dissipates, however, your child should calm down. If this isn’t the case, let the doctor know.
- There’s an Obvious Deformity. If your child’s leg looks like it’s at a weird angle after the fall, it might be broken. In this case, call the doctor and be prepared to go to the ER.
Insider Info:
A simple X-ray is usually enough to diagnose a lower extremity fracture. Fractures aren’t always picked up on the initial X-ray, however, which can be frustrating. Sometimes there’s a lag. If your child continues to complain of pain or has a persistent limp despite a negative X-ray, let the doctor know. In this case, the x-ray may need to be repeated.
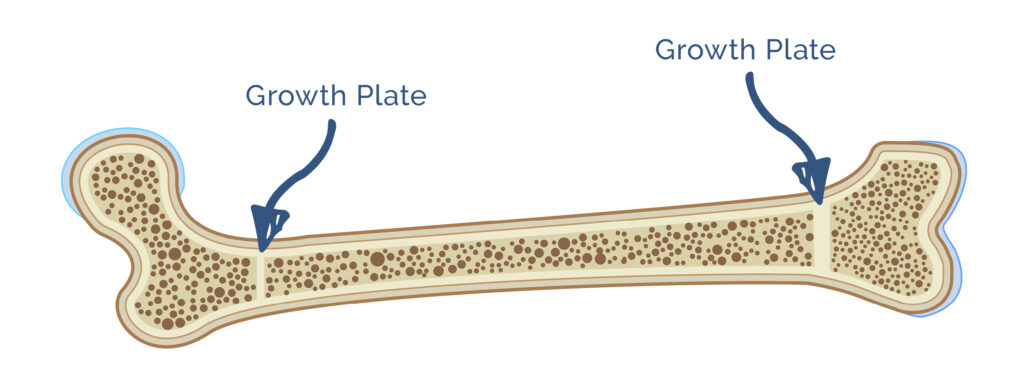
Because children are still growing, they’re at risk for “growth plate” fractures.
What are Growth Plates? Growth plates are areas of cartilage found at the ends of bones. Growth plates are important because they allow bones to grow longer. After a child goes through puberty, their growth plates fuse, signaling they’re done growing.
If a growth plate breaks, the bone may grow abnormally. Because of this, the early diagnosis of fractures (through imaging) is critical.
Cuts & How to Manage Them
Most cuts and scrapes are minor and heal on their own.
If Your Child Gets a Cut and It’s Bleeding, Do the Following:
1. “Hold pressure” (with a tissue or a piece of toilet paper) to stop the bleeding.
2. Clean the cut with soap and water.
4. After you’ve examined the cut, it becomes a choose your own adventure story based on what the cut looks like:
Option #1: If the cut is minor, apply an anti-bacterial ointment (such as Neosporin) to the affected area and cover it with a Band-Aid.
Insider Info: Back in the day, doctors recommended “drying out” cuts, thinking they healed better and faster when left exposed to the air. Now, studies show that keeping cuts moist and covered is the way to go.1
PediaTip: Check the cut daily to make sure that it’s not getting infected.
Option #2: If the cut looks worrisome, your child may need stitches. In this case, call the doctor.
Medical Attention is Usually Needed for the Following:
- The Cut is Deep and Gaping. These types of cuts often require stitches.
Insider Info: The depth of a cut can be hard to assess, so err on the side of caution and call the doctor if you’re not sure. If you see globs of fat oozing out of the cut, you know that it’s deep.
- The Cut Won’t Stop Bleeding Even Though You’ve Been “Holding Pressure” for 10-Plus Minutes.
- The Wound is in a Tricky Location. Lacerations in the following areas may need to be sutured by a plastic surgeon for cosmetic reasons (i.e. so they look pretty when they heal) and to prevent complications.
- Cuts in the upper part of the ear.
- Cuts through the upper or lower borders of the lip (fancy name: the vermilion borders). Cuts ON the lip itself don’t usually require stitches.
- Cuts at the hairline.
- Cuts that run across the eyebrow.
- Cuts in the nasal septum (the cartilage that divides the two nostrils).
- Eyelid cuts.
Insider Info: It’s rare to need stitches on the tongue or the gums. Why? Because these areas tend to heal well without stitches (unless the tongue is cut all the way through, which it’s usually not).
- The Wound Starts to Get Infected (i.e. it starts to ooze pus, turns red, becomes painful, or your child spikes a fever).
- The Cause of the Cut (i.e. the Mechanism of Injury) Makes It More Likely That the Cut is Going to Get Infected (i.e. That It’s a “Dirty” Wound). Animal bites, human bites, and cuts from a rusty nail are all considered “dirty” wounds.
- Your Child’s Immunizations Aren’t Up To Date. In this case, your child may need a tetanus booster.
- For “clean” wounds, a tetanus booster is recommended if the child has gotten fewer than 3 doses of the tetanus vaccine OR if the most recent tetanus shot was given 10+ years ago.
- For “dirty” wounds, a tetanus booster is needed if the child has gotten fewer than 3 doses of the tetanus vaccine OR it’s been 5+ years since the last tetanus shot.
Not Sure if Your Child’s Tetanus Series is Current (or Adequate)? Ask their doctor. Know too, that kids usually get tetanus shots at 2 months, 4 months, 6 months, 15 months, and again at 4 years. They get an additional tetanus booster shot between 11-12 years and a tetanus booster every 10 years after that.
PediaTip: If you’re concerned about your child’s cut, don’t wait to seek treatment. Why Not? Because it’s best to get stitches within 12 hours of the injury, ideally within 6-8 hours. After that, the risk of infection goes way up.
If the doctor thinks your child needs stitches based on the clues above, they’ll tell you where to go.
The Options Are: The doctor’s office, a plastic surgeon’s office, the ER, or an urgent-care center with doctors well-versed in pediatrics.
Insider Info: Stitches Aren’t the Only Game in Town.
- Glue (e.g. Dermabond) and Steri-strips (butterfly bandage closures) can be used for small, straightforward cuts.
- Staples are commonly used for cuts on the scalp. Although head wounds tend to bleed a lot, only a few staples are usually needed to close them. Don’t worry, the doctor isn’t pulling out their office stapler for this; a fancy staple gun is used instead. Although putting staples in a child’s head sounds kind of barbaric, they go in fast and do the job well.
Get Wise About Additional Questions That Parents Tend to Have About Stitches.
The 411 on Human Bites & Animal Bites
Animal bites and human bites can get infected and must be taken seriously even if they don’t look all that bad.
PediaTrivia:
- Human bites are the dirtiest type of bite (i.e. they have the highest concentration of bacteria).
- Cat bites are more likely to get infected, though, because they go so deep.
- Dog bites have the potential to get infected, as well, and tend to vary in their severity.
How are Bites Managed?
All injuries from bites need to be irrigated (washed out with water). If the teeth break your child’s skin, call the doctor. Minor bites can probably be managed at home (with thorough cleaning of the wound), but more significant bites need to be seen in the doctor’s office or in the ER. Why? Because doctors can more thoroughly irrigate the wound and start antibiotics if needed.
Insider Info: An animal bite may not be stitched up immediately (or at all) because of the high risk of infection.
A Word About Rabies
What is Rabies?
It’s a disease caused by the rabies virus. Humans contract it when they’re bitten or scratched by a rabid animal.
What’s So Bad About Rabies?
Rabies is super rare, but it can be fatal if it’s not treated promptly or properly.
Which Animals Carry Rabies?
The most common rabies-carrying culprits in the U.S. are bats, raccoons, skunks, and foxes.
Why Aren’t Dogs On This List?
Because most dogs in the U.S. get the rabies vaccine. It’s a different story abroad, however, so be extra careful if you or your child gets bitten by a dog in a foreign country.
Insider Info:
- Bats are particularly worrisome carriers of rabies because their bite is so soft that a parent might not even realize their child had been bitten. Therefore, doctors advise parents to seek care even if their child is merely in the same room as a bat.
Although there are only 1-3 human rabies cases reported in the U.S. each year, 70% of rabies deaths in the U.S. are caused by bats.2
- Chipmunks, gerbils, guinea pigs, hamsters, mice, rats, rabbits, moles, and gophers rarely carry rabies and haven’t been known to cause any human rabies cases in the U.S. Squirrels are almost always rabies-free, as well. If a crazed squirrel bites your child, though, call the doctor, just to be safe. Most squirrels won’t come near you, however, and are happily burying their nuts and forgetting where they put them.
PediaTrivia:
Gray squirrels find only 26% of the nuts they bury.3
What are the Symptoms of Rabies?
For the rabies virus to cause symptoms, it needs to travel from the site of the bite to the brain. If treatment is sought early enough, medication may be able to stop the virus in its tracks. Once the symptoms appear, though, it’s often too late.
Rabies Symptoms Include (But Aren’t Limited To):
- Flu-like symptoms
- Anxiety
- Confusion
- Agitation
- Insomnia
- Strange behavior
- Hallucinations
- Hydrophobia (a fear of water)
If Your Child is Bitten By a Potentially Rabid Animal, Take the Following Steps:
1. If the animal is a pet, ask the owner if their furry friend’s shots are up to date. If the animal isn’t a pet, call animal control to see if it can be captured and observed for rabies.
2. Call the doctor. If the doctor is worried, they’ll send your child to the ER.
3. If the ER doctor is concerned about rabies, they’ll recommend rabies “PEP,” which stands for “post-exposure prophylaxis.” Although rabies PEP isn’t fun to get, it can be lifesaving. With rabies PEP, kids receive 5 shots over 14 days. One of the shots is a dose of immune globulin, while the other 4 are single doses of the rabies vaccine.
Reality Check: It’s much more likely that an animal bite will get infected than lead to rabies.
The Bottom Line: Reach out to the doctor if your child is bitten by a human or an animal.
Splinters & How to Remove Them
Now, let’s downshift to a less intense topic: splinters.
Splinters are common in kids and can often be managed at home. Here are the steps to safely remove a splinter at home:
1. Clean the area with soap and water.
2. Grab one end of the splinter with tweezers and pull gently.
3. If you can’t get the splinter out, that’s okay. Don’t go digging around for it. Probing the area will only increase the risk of infection. Plus, it will make your child mad! Remember, your child’s body sees splinters as foreign objects and wants to get them out as much as you do.
4. If the splinter isn’t budging OR an infection seems to be brewing (e.g. there’s redness, pain, or pus at the site of the splinter), have the pediatrician remove it.
The Bottom Line
Cuts, scrapes, and falls are an inevitable part of growing up. To help you prepare for them, here are the Top 15 items to include in your first-aid kit:
- Band-Aids.
- Elastic Wrap Bandages.
- Athletic Tape.
- An Instant Cold Compress (aka an ice pack).
- Alcohol Wipes (to clean cuts and remove residue from Band-Aids and athletic tape).
- Hydrogen Peroxide (you can pour hydrogen peroxide onto cuts to disinfect them).
- Eyewash Solution.
- Vaseline.
- Neosporin (an anti-bacterial ointment for cuts and scrapes).
- Calamine Lotion.
- Tylenol and ibuprofen.
- Benadryl. Benadryl is typically reserved for children 2 years and older when it’s used for (minor) allergic reactions and is often limited to kids 6 years and older when it’s used as a decongestant (unless the doctor recommends otherwise). If your child has an Epi-Pen, add it to the kit as well.
- 1% Hydrocortisone cream (a steroid cream).
- A Thermometer.
- Scissors and Tweezers.
For serious falls and injuries that require more than what’s in your first-aid kit, call the doctor.
Whew…That Was a Lot of Info. And Breathe….
And Now for a Quote…
“Even when freshly washed and relieved of all obvious confections,
children tend to be sticky.”
The Reminders for This Week are the Same as Last Week’s. Get Wise About Them Below…
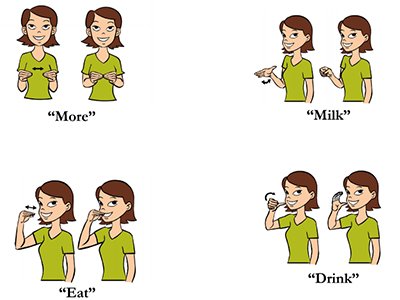
- Limit Your Child’s Whole Milk to 16-24 Ounces Per Day.
- Feed Your Child What You Eat, But Cut into Small Pieces.
- Steer Clear of Choking Hazards. Get Wise About the Top 10 (Food) Choking Hazards Here.
- Brush Your Child’s Teeth Twice a Day (Especially After the Last Meal of the Night) and Have Them Visit the Dentist Every 6 Months (Unless the Dentist Says Otherwise).
- Call the Doctor If Your Child Spikes a Fever Above 102.2°F OR If They Develop Any Other Worrisome Symptoms (Such as Lethargy or Poor Feeding).
- Continue to Give Your Child a Daily Vitamin D Supplement (600 International Units Per Day).
- Keep Your Child in a Rear-Facing Car Seat Until (At Least) 2 Years of Age.